Neulasta (pegfilgrastim) is prescribed to help prevent serious infection from chemotherapy for certain cancers, and from a certain form of radiation sickness. It’s a biologic drug that comes as an injection and a skin patch.
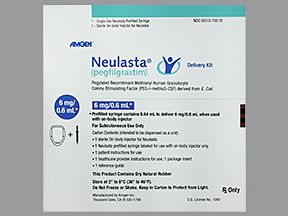
Neulasta is a brand-name prescription medication. It comes as a liquid solution that’s given as an injection in one of two ways:
- From a syringe. For these injections, Neulasta prefilled syringes are used. And the drug is given as an injection under your skin. Your healthcare professional will give you Neulasta injections. Or, they’ll teach you how to self-inject the drug at home.
- Through a special type of skin patch. For delivery by skin patches, Neulasta Onpro is used. It’s a special type of patch called an on-body injector. Your healthcare professional will prepare the Neulasta Onpro patch. Then they’ll attach it to your body on the day you receive chemotherapy. About a day later, Neulasta gets delivered through the patch into your body as an injection under your skin.
Neulasta is used to help prevent infections in adults and some children. However, the Neulasta Onpro patch isn’t used in children or to treat radiation sickness. It’s only used in adults taking certain chemotherapy drugs that increase the risk of serious infections.
Neulasta is a biologic medication, which means it’s made from living organisms. It’s a lab-created copy of a hormone that’s made naturally by your body. Neulasta is available in biosimilar forms. Biosimilars are like generic drugs. But unlike generics, which are made for nonbiologic drugs, biosimilars are made for biologic drugs.
Read on to learn about Neulasta’s side effects, cost, and more. And to learn more about Neulasta’s uses, see the “What is Neulasta used for?” section below.
Like most drugs, Neulasta may cause mild or serious side effects. The lists below describe some of the more common side effects that Neulasta may cause. These lists don’t include all possible side effects.
Keep in mind that side effects of a drug can depend on:
- your age
- other health conditions you have
- other medications you may be taking
Your doctor or pharmacist can tell you more about the potential side effects of Neulasta. They can also suggest ways to help reduce side effects.
Mild side effects
Here’s a short list of some of the mild side effects that Neulasta can cause. To learn about other mild side effects, talk with your doctor or pharmacist, or read Neulasta’s patient information.
Mild side effects* of Neulasta that have been reported include:
- pain in your arms or legs
- pain or tenderness at Neulasta injection sites
- bone pain
- skin-related side effects, with use of Neulasta Onpro patch
Mild side effects of many drugs may go away within a few days or a couple of weeks. But if they become bothersome, talk with your doctor or pharmacist.
* For more information on these side effects, see the “Side effect focus” section below.
Serious side effects
Less commonly, some people develop serious side effects with Neulasta. If you have serious side effects from Neulasta, call your doctor right away. But if you think you’re having a medical emergency, you should call 911 or your local emergency number.
Serious side effects of Neulasta that have been reported include:
- increased levels of white blood cells, which can be a sign of infection and may cause fever, bleeding or bruising, and trouble breathing
- aortitis (inflammation of the aorta, the heart’s main artery), which may cause fever, feeling tired, back spasms or pain, and belly pain
- acute respiratory distress syndrome (a lung condition that causes you to suddenly have trouble breathing)
- capillary leak syndrome (a condition in which there’s leakage from tiny blood vessels called capillaries)
- kidney problems such as glomerulonephritis (inflammation of a certain part of your kidneys)
- allergic reaction*
* For more information on these side effects, see the “Side effect focus” section below.
Side effect focus
If you’re taking Neulasta, you may be wondering how long side effects of Neulasta last, or maybe you’re looking for advice on how to deal with Neulasta’s side effects. Read on to learn details about some of the side effects Neulasta may cause. You can see also see this in-depth article for more information about Neulasta’s side effects.
Bone pain
The most common side effect of Neulasta is bone pain. And it typically affects your back and legs.
You may be wondering how long this bone pain lasts. For most people, it starts within 2 days of receiving the drug. The duration of bone pain from Neulasta is usually 2 to 4 days.
What might help
Over-the-counter (OTC) medications are usually effective in preventing or relieving bone pain from Neulasta. Some examples of these drugs include:
- acetaminophen (Tylenol)
- ibuprofen (Advil, Motrin)
- naproxen (Aleve)
There’s some
If you’re unsure about which OTC medications are best for you, talk with your doctor or pharmacist. And be sure to check with them before starting any medications while you’re taking Neulasta.
If your bone pain doesn’t go away or becomes severe, tell your doctor. They may recommend certain prescription medications, such as corticosteroids or opioids. Or, they may recommend changes to your overall treatment plan.
Pain with Neulasta injections
It’s common to get pain in your arms or legs from Neulasta injections. For some people, this can be a throbbing pain. But the pain usually goes away within a few days after your dose of Neulasta has been given.
Some people also have injection site side effects from Neulasta. These side effects occur around the site where the drug was injected. And they can cause the following:
- pain
- tenderness
- stinging
- swelling
- skin irritation
What might help
Pain in your arms or legs from Neulasta injections can usually be eased by OTC pain medications. Some examples of these drugs include:
- acetaminophen (Tylenol)
- ibuprofen (Advil, Motrin)
- naproxen (Aleve)
If you’re not sure which OTC pain medication is best for you, ask your doctor or pharmacist. Be sure to check with them before starting any medications while you’re taking Neulasta.
If you’re injecting Neulasta doses yourself at home, take the prefilled syringe of the drug out of the refrigerator at least 30 minutes before your injection. Doing so may help to lessen stinging when you inject your dose.
Using a warm or cool compress after your injection may also help ease injection site side effects such as swelling or skin irritation.
If you have pain that becomes severe or doesn’t go away, tell your doctor. They may prescribe other medications to ease your pain or recommend changes to your treatment plan.
Side effects of Neulasta patches
If you use Neulasta Onpro patches, your healthcare professional will prepare and apply the patch for you.
Although it isn’t known how often they occur, some people have had the following patch application site side effects:
- bleeding
- bruising
- pain
- redness or deepening of skin color
Also, keep in mind that some people are sensitive to adhesives. Both mild and serious allergic reactions to the acrylic adhesive in Neulasta Onpro patch have happened. Symptoms of this type of reaction may include:
- skin rash
- itching
- hives
For more information about allergic reaction to Neulasta itself, see the “Allergic reaction” section directly below.
What might help
Application site side effects from Neulasta Onpro patches usually go away on their own within a few days.
But if you have symptoms of an allergic reaction to either the drug or its adhesive, you should remove the patch right away. Then, call your doctor and let them know what happened.
If your allergic reaction feels severe, call 911 or your local emergency number. See the section just below for symptoms of a severe allergic reaction.
Allergic reactionSome people may have an allergic reaction to Neulasta. It isn’t known how often allergic reactions occur with Neulasta.
Symptoms of a mild allergic reaction can include:
- skin rash
- itchiness
- flushing (temporary warmth, redness, or deepening of skin color)
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include swelling under your skin, typically in your eyelids, lips, hands, or feet. They can also include swelling of your tongue, mouth, or throat, which can cause trouble breathing.
Allergic reactions from Neulasta usually happen the first time you take the drug. So, it’s best to have a family member or caregiver nearby for at least 1 day after you receive your first dose.
Neulasta Onpro patches contain acrylic adhesive, which some people can be allergic to. If you have an allergic reaction while you’re wearing a Neulasta Onpro patch, immediately grab the edge of the adhesive pad and peel off the patch.
Call your doctor right away if you have an allergic reaction to Neulasta. If you think you’re having a medical emergency, call 911 or your local emergency number.
Find answers to some commonly asked questions about Neulasta.
Is Neulasta similar to either Neupogen or Udenyca?
Neulasta is similar to both Neupogen and Udenyca. Neulasta, Neupogen, and Udenyca all belong to the same group of drugs called G-CSF agents.
G-CSF stands for granulocyte colony-stimulating factor. It’s made naturally by your body. Its purpose is to signal your bone marrow to make more neutrophils. Neutrophils are a type of white blood cell that works to fight infections.
All G-CSF agents (including Neulasta, Neupogen, and Udenyca) mimic the effects of G-CSF. These drugs make your body produce more neutrophils.
These medications are used to help prevent febrile neutropenia. With this serious type of infection, you have a low level of neutrophils and a fever. They’re given to people who are taking certain cancer treatments that increase the risk of infection.
Here’s a summary of the active drugs in these medications and how they’re taken:
- Neulasta. Neulasta contains the active drug pegfilgrastim. Its effects last longer than Neupogen’s do. Neulasta only has to be taken once during each chemotherapy cycle.
- Neupogen. Neupogen contains the active drug filgrastim. It was the first drug made in this group of drugs, and it was approved in 1991. With Neupogen treatment, you’ll usually need a daily injection for 10 days for the drug to be effective.
- Udenyca. Udenyca is a biosimilar of the brand-name drug Neulasta. Biosimilars are like generic drugs. But unlike generics, which are made for nonbiologic drugs, biosimilars are made for biologic drugs. Biologic drugs are made from living organisms rather than from chemicals. Udenyca contains the active drug pegfilgrastim-cbqv. The dosing schedule for Udenyca is similar to that of Neulasta. It’s taken once per chemotherapy cycle.
When will Neulasta reach its peak effect in my body? And how long will it last in my system?
Neulasta begins working shortly after it’s given. Its peak (strongest) effect occurs around 16 hours to 5 days after you receive a dose.
The drug’s effects last for about 1 to 2 weeks in your system.
Should I take Claritin before or while receiving Neulasta?
Some
If you’re concerned about bone pain with Neulasta, talk with your doctor about whether you should take Claritin.
Claritin doesn’t usually cause negative side effects. So for most people, it’s worth a try to help reduce bone pain. But be sure to check with your doctor before taking any medications with Neulasta.
How does Neulasta work?
Neulasta belongs to a group of drugs called G-CSF agents. G-CSF stands for granulocyte colony-stimulating factor.
G-CSF is made naturally by your body. Its purpose is to stimulate your bone marrow to make neutrophils. Neutrophils are a type of white blood cell that work to fight off infections.
Neulasta works by mimicking the effects of G-CSF. It signals your bone marrow to make more neutrophils.
Some cancer treatments (including certain chemotherapy drugs or radiation) cause many side effects. And these side effects may include altering your body’s natural production of neutrophils.
If you’re receiving certain cancer treatments, you have an increased risk for serious infections, which can sometimes be life threatening.
Neulasta can help reduce your risk for serious infections. It does this by increasing your level of neutrophils, helping to boost your immune system’s ability to fight off infections.
How can I know when Neulasta Onpro is done administering the drug to me?
Neulasta Onpro patch is an on-body injector (OBI) that’s designed to automatically deliver your dose of Neulasta. It gives the dose to you over a 45-minute period.
The OBI device will begin to administer Neulasta to you about 27 hours after your doctor applies the patch to your skin. They’ll apply the patch on the day you receive chemotherapy.
There are three ways to know when Neulasta Onpro is done administering the drug to you:
- Hear the beep. The Neulasta Onpro patch will beep before and after it delivers your dose.
- See the indicator light stop flashing. The Neulasta Onpro patch has an indicator that’ll change from a flashing green light to a solid green light, and then it’ll turn off once your dose has been given.
- See the empty fill window. There’s a small window on the Neulasta Onpro patch that shows the medication level inside the device. The level will move from the “full” line to the “empty” line once your dose has been given.
For more details on using Neulasta Onpro, you can view instructions for use on the manufacturer’s website.
Costs of prescription drugs can vary depending on many factors. These factors include what your insurance plan covers and which pharmacy you use.
Biosimilars are like generic drugs. But unlike generics, which are made for nonbiologic drugs, biosimilars are made for biologic drugs such as Neulasta. And sometimes, biosimilars are less expensive than their parent drugs.
Examples of available biosimilars for Neulasta include:
- pegfilgrastim-bmez (Ziextenzo)
- pegfilgrastim-cbqv (Udenyca)
- pegfilgrastim-jmdb (Fulphila)
If you have questions about how to pay for Neulasta, talk with your doctor or pharmacist. You can also visit the Neulasta manufacturer’s website to see if they have support options.
Your doctor will recommend the dosage of Neulasta that’s right for you. Below are commonly used dosages, but always take the dosage your doctor prescribes.
Forms and strength
Neulasta comes as a liquid solution that’s given as an injection one of two ways:
- From a syringe. For these injections, Neulasta prefilled syringes are used. And the drug is given as an injection under your skin. Your healthcare professional will give you Neulasta injections, or they’ll teach you how to self-inject the drug at home.
- Through a special type of skin patch called Neulasta Onpro. The patch contains an on-body injector (OBI). Your healthcare professional will fill the OBI using a prefilled syringe that contains the liquid Neulasta medication. Then, they’ll attach it to your belly or the back of your arm on the day you receive chemotherapy. About 27 hours later, the drug will be delivered into your body as an injection under your skin through a small cannula (a small, short tube).
Neulasta comes in one strength: 6 milligrams (mg) per 0.6 milliliter (mL).
Note: Neulasta Onpro patch is only used in adults taking treatment with certain chemotherapy drugs that increase the risk of serious infection. It’s not used in people with radiation sickness or in children. To learn more about Neulasta’s uses, see the “What is Neulasta used for?” section below.
Recommended dosages
How often you’ll take Neulasta depends on your condition.
For example, if you’re using the drug to prevent serious infections during chemotherapy, you’ll take Neulasta once each chemotherapy cycle. But the drug won’t be given in the 14 days before or the 24 hours after your chemotherapy dose is given.
But, if you’re using the drug for radiation sickness, you’ll take two doses, which are given 1 week apart.
Questions about Neulasta’s dosage
Here are some common questions related to Neulasta’s dosage.
- What if I miss a dose of Neulasta? If you miss a dose of Neulasta, call your doctor as soon as possible. They can recommend when you should self-inject your missed dose or if you’ll need to reschedule an appointment to get your dose.
- Will I need to use Neulasta long term? Yes, you’ll need to use Neulasta long term. You’ll likely continue using the drug for as long as you’re receiving chemotherapy or experiencing radiation sickness. Your doctor will tell you when it’s safe for you to stop Neulasta treatment.
- How long does Neulasta take to work?
Studies show that it may take 1 to 2 weeks for your neutrophil level to return to normal after taking Neulasta following a round of chemotherapy. Neutrophils are a type of white blood cell that work to fight off infections. The drug’s effects last in your system for about 1 to 2 weeks.
Your doctor will explain how Neulasta will be given to you. They’ll also explain how much you’ll receive and how often. Be sure to follow your doctor’s instructions.
Receiving Neulasta
Neulasta comes as a liquid solution that’s injected under your skin. This is done using either a prefilled syringe or a special type of skin patch.
If you’re receiving Neulasta by injection with a syringe, your healthcare professional may give you injections. Or they may teach you how to self-inject the drug at home.
If you’re using a Neulasta Onpro skin patch, your healthcare professional will prepare the patch. The patch contains an on-body injector (OBI) with a small cannula (a small, short tube). Your healthcare professional will fill the OBI with the liquid Neulasta medication. They’ll then attach the OBI to your body on the day you receive chemotherapy.
Your healthcare professional might place the patch on your belly or the back of your arm. About 27 hours later, the drug will be delivered into your body as an injection under your skin through the cannula.
Receiving Neulasta with other drugs
Neulasta is given as part of a cancer treatment plan that includes other drugs.
In fact, Neulasta is commonly used with chemotherapy to help with a common side effect of chemotherapy: increased risk of infection.
If you have questions about any other drugs you’ll be taking with Neulasta, talk with your doctor.
Taking Neulasta with food
Neulasta is given as an injection under your skin. So, how well Neulasta works doesn’t depend on when you eat, but your chemotherapy drug may be affected by food. Talk with your doctor to see when it’s best to eat considering your overall treatment plan.
Questions for your doctorYou may have questions about Neulasta and your treatment plan. It’s important to discuss all your concerns with your doctor.
Here are a few tips that might help guide your discussion:
- Before your appointment, write down questions like:
- How will Neulasta affect my body, mood, or lifestyle?
- Bring someone with you to your appointment if doing so will help you feel more comfortable.
- If you don’t understand something related to your condition or treatment, ask your doctor to explain it to you.
Remember, your doctor and other healthcare professionals are available to help you. And they want you to get the best care possible. So, don’t be afraid to ask questions or offer feedback on your treatment.
Your doctor may prescribe Neulasta for you if you have an increased risk for serious infections. This may be the case if you:
- take a chemotherapy drug that puts you at risk for a serious infection called febrile neutropenia (a low level of white blood cells called neutrophils plus a fever), or
- have a certain form of radiation sickness called hematopoietic subsyndrome
Neulasta is used in adults and children to prevent serious infections for the reasons listed above.
Chemotherapy drugs and radiation are used to treat cancer. But cancer treatments can have many side effects, including increased risk of infection. However, there are many ways to help prevent or reduce some of these side effects.
To learn how Neulasta works for these conditions, see “How does Neulasta work?” in the “What are some frequently asked questions about Neulasta?” section above. And keep reading to learn more about the conditions themselves.
Using Neulasta while taking chemotherapy
Chemotherapy drugs work by killing cancer cells. But, as a side effect, chemotherapy drugs also destroy healthy cells like neutrophils. Neutrophils are white blood cells that work to protect your body from infection.
Neutropenia (a low level of neutrophils) is a common side effect of certain chemotherapy drugs. With febrile neutropenia, you have a fever and neutropenia. A fever is often a sign of infection.
Febrile neutropenia is a serious condition and can possibly lead to death. So, if you develop a fever while you’re taking cancer treatments, let your doctor know right away.
Neulasta is used to help prevent neutropenia in people who’re receiving certain cancer treatments. The drug helps to reduce the risk of serious infections during cancer treatment.
For example, if you have breast cancer and receive the chemotherapy drug carboplatin, your doctor may prescribe Neulasta. You’ll receive a dose of Neulasta after chemotherapy, at least 24 hours after each round.
Using Neulasta for radiation sickness
Neulasta is also used to treat hematopoietic subsyndrome of acute radiation syndrome, which is a certain form of radiation sickness.
With radiation sickness, you can develop problems with your stem cells. Stem cells are cells in your bone marrow that develop into different types of cells, including white blood cells such as neutrophils.
Radiation sickness may cause the following symptoms:
Without enough white blood cells, you can become seriously ill from infections that your body would normally fight off with ease.
Neulasta may also be used off-label for other conditions. With off-label use, a drug that’s approved for certain conditions is prescribed for a different reason. Talk with your doctor for more information.
Neulasta contains the drug pegfilgrastim, which is a biologic medication. A biologic medication is made from living organisms. Fulphila contains the active drug pegfilgrastim-jmdb, and it’s a biosimilar form of Neulasta.
Biosimilars are like generic drugs. But unlike generics, which are made for nonbiologic drugs, biosimilars are made for biologic drugs.
For more information, see this side-by-side comparison of Neulasta and Fulphila. Also, be sure to talk with your doctor about which medication is right for you.
Neulasta and Granix belong to the same group of drugs called G-CSF agents.
G-CSF stands for granulocyte colony-stimulating factor. It’s made naturally by your body, and it works by signaling your bone marrow to make neutrophils. Neutrophils are a type of white blood cell that work to fight off infections.
Granix (tbo-filgrastim) is a biosimilar version of another drug called Neupogen (filgrastim). Biosimilars are like generic drugs. But unlike generics, which are made for nonbiologic drugs, biosimilars are made for biologic drugs. Granix has to be given once daily to be effective.
Neulasta contains the active drug pegfilgrastim. Neulasta’s effects last longer than either Granix’s or Neupogen’s do. To be effective, it only has to be given once during each chemotherapy cycle.
To learn more about these drugs, view this detailed breakdown. Check with your doctor to see which treatment is right for your condition.
There aren’t any known interactions between Neulasta and other drugs, herbs and supplements, or foods. An interaction occurs when medications, vaccines, foods, and other substances affect how a certain drug works.
To be safe, let your doctor know about all medications you take, including prescription and over-the-counter types. Also describe any vitamins, herbs, or supplements you use. Your doctor or pharmacist can tell you about any interactions these items may cause with Neulasta.
If you have any questions about possible interactions with Neulasta, talk with your doctor or pharmacist.
Neulasta may not be right for you if you have certain medical conditions or other factors that affect your health. Talk with your doctor about your health history before you take Neulasta. They can recommend if this drug is safe for you to take. Factors to consider include those in the list below.
- Certain blood cancers. If you have myeloid cancer (cancer that affects the bone marrow), you shouldn’t take Neulasta. This drug could cause your cancer to get worse, so it’s important to talk with your doctor about other treatment options.
- Allergic reactions. If you’ve ever had an allergic reaction to Neulasta or any of its ingredients, including acrylics, adhesives, or latex, you shouldn’t take Neulasta. Ask your doctor what other medications are better options for you.
- Sickle cell disorder. If you have a sickle cell disorder, taking Neulasta can cause sickle cell crisis, which can be life threatening. Sickle cell disorder affects your red blood cells. Tell your doctor if you have sickle cell disorder.
There aren’t any known interactions between Neulasta and alcohol. But, alcohol could worsen some side effects of certain chemotherapy drugs. And Neulasta is commonly used with chemotherapy.
If you have questions about drinking alcohol while taking Neulasta, talk with your doctor.
It isn’t known if Neulasta is safe to take during pregnancy or while breastfeeding.
If you’re pregnant or breastfeeding, or considering either, talk with your doctor before starting Neulasta. They’ll recommend the best treatment plan for you during this time.
Do not take more Neulasta than your doctor prescribes. Using more than this can lead to serious side effects.
Symptoms of overdose
Symptoms caused by a Neulasta overdose can include:
What to do in case you take too much Neulasta
Call your doctor if you think you’ve taken too much Neulasta. You can also call 800-222-1222 to reach the American Association of Poison Control Centers, or use its online resource. If you have severe symptoms, immediately call 911 or your local emergency number, or go to the nearest emergency room.
If you have radiation sickness or take chemotherapy drugs that increase your risk for serious infection, your doctor may recommend Neulasta. To read more about these uses, see the “What is Neulasta used for?” section above.
You can learn more about ways to prevent infections in this article. Also, you can learn about chemotherapy’s side effects to help you know what to expect during treatment.
If you have questions about Neulasta, talk with your doctor or pharmacist. If you’re unsure what to ask, here are some questions to help you get the conversation started:
- Where and when will I receive my Neulasta treatments?
- Is there anything I should do to prepare for my first Neulasta dose?
- Do my other medications increase my risk for side effects with Neulasta?
- What over-the-counter medications should I take to help lower my risk for side effects of Neulasta, and when should I take them?
To learn more about Neulasta, see this article:
To get information on different conditions and tips for improving your health, subscribe to any of Healthline’s newsletters. You may also want to check out the online communities at Bezzy. It’s a place where people with certain conditions can find support and connect with others.
Q:
Is it safe for me to receive vaccines while I’m taking Neulasta?
AnonymousA:
It depends on the type of vaccine you’ll be receiving and your risk for infection.
If you’re using Neulasta to increase your level of neutrophils, you shouldn’t get any live vaccines. Neutrophils are a type of white blood cell that work to fight off infections.
Live vaccines contain a weakened form of a germ that causes a certain infection. When your neutrophils are low, a live vaccine could give you the infection instead of protecting you from it.
Examples of live vaccines include:
- measles, mumps, rubella (MMR)
- intranasal influenza (flu vaccine that’s given in your nose)
There are other types of vaccines available, too. For instance, inactivated vaccines contain a form of a germ that’s no longer alive. Examples of inactivated vaccines include:
Another type of vaccine is called a messenger RNA (mRNA) vaccine. Once inside your body, this type of vaccine makes proteins to trigger a certain immune response. Some COVID-19 vaccines use this type of formulation.
It’s generally recommended that you wait at least 2 weeks after receiving chemotherapy before getting an inactivated or mRNA vaccine. Keep in mind that Neulasta is commonly used with chemotherapy.
If you’re interested in receiving any vaccines, talk with your doctor. They can recommend if it’s safe for you to receive a vaccine while you’re taking Neulasta.
The Healthline Pharmacist TeamAnswers represent the opinions of our medical experts. All content is strictly informational and should not be considered medical advice.Disclaimer: Healthline has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.