If you have psoriasis, your doctor may recommend treatment with Ilumya.
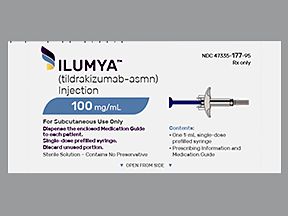
Ilumya is a brand-name prescription medication used in adults with moderate to severe plaque psoriasis.
To learn more, see the “Is Ilumya used for plaque psoriasis?” section below.
Ilumya basics
Ilumya comes as a liquid solution inside prefilled syringes. You’ll receive Ilumya as an injection under the skin at your doctor’s office or another healthcare facility.
Ilumya contains the active drug tildrakizumab-asmn. (An active drug is an ingredient that makes a medication work.)
Tildrakizumab-asmn is a type of biologic medication. A biologic is made from parts of living organisms. Ilumya is not available in a biosimilar form. (Biosimilars are like generic drugs. But unlike generics, which are made for non-biologic drugs, biosimilars are made for biologic drugs.) Instead, tildrakizumab-asmn is only available as the brand-name drug Ilumya.
This article provides information about Ilumya’s side effects, cost, dosage, and more.
Like most drugs, Ilumya injections may cause mild or serious side effects. The lists below describe some of the more common side effects that Ilumya may cause. These lists don’t include all possible side effects.
Keep in mind that the side effects of a drug can depend on:
- your age
- other health conditions you have
- other medications you take
Your doctor or pharmacist can tell you more about the potential side effects of Ilumya. They can also suggest ways to help reduce side effects.
Mild side effects
Here’s a short list of some of the mild side effects that Ilumya can cause. To learn about other mild side effects, talk with your doctor or pharmacist, or read Ilumya’s prescribing information.
Mild side effects of Ilumya that have been reported include:
- diarrhea
- injection site reactions
- upper respiratory infection, such as the common cold
Mild side effects of many drugs may go away within a few days to a couple of weeks. But if they become bothersome, talk with your doctor or pharmacist.
Serious side effects
Serious side effects from Ilumya can occur, but they aren’t common. If you have serious side effects from Ilumya, call your doctor right away. But, if you think you’re having a medical emergency, you should call 911 or your local emergency number.
Serious side effects of Ilumya that have been reported include:
- serious infection
- allergic reaction
Allergic reactionSome people may have an allergic reaction to Ilumya. These reactions were reported in Ilumya’s clinical studies. It’s unknown how often they occurred in these studies.
Symptoms of a mild allergic reaction can include:
A more severe allergic reaction is possible. Symptoms of a severe allergic reaction can include swelling under your skin, typically in your eyelids, lips, hands, or feet. They can also include swelling of your tongue, mouth, or throat, which can cause trouble breathing.
Call your doctor right away if you have an allergic reaction to Ilumya. But if you think you’re having a medical emergency, call 911 or your local emergency number.
Costs of prescription drugs can vary depending on many factors. These factors include what your insurance plan covers and which pharmacy you use.
If you have questions about how to pay for your prescription, talk with your doctor or pharmacist. You can also visit the Ilumya manufacturer’s website to see if they have support options.
You can also check out this article to learn more about saving money on prescriptions.
Your doctor will recommend the Ilumya dosing that’s right for you. Below are commonly used dosages, but your doctor will determine the dosage you’ll receive.
Form
Ilumya comes as a liquid solution inside prefilled syringes. You’ll receive Ilumya as an injection under the skin at your doctor’s office or another healthcare facility.
Recommended dosage
To start, you’ll receive one Ilumya injection, then another injection 4 weeks later. After that, you’ll get an Ilumya injection every 12 weeks.
If you miss an appointment to get an Ilumya injection, call your doctor as soon as possible. They’ll help reschedule your appointment to receive Ilumya.
Questions about Ilumya’s dosage
Below are some common questions about Ilumya’s dosage.
- Will I need to use Ilumya long term? Yes. If you and your doctor agree that Ilumya is safe and working for you, you’ll likely take the drug long term.
- How long does Ilumya take to work? Ilumya begins working as soon as you take a dose. But it may be several weeks before you notice it easing your psoriasis symptoms.
Find answers to some commonly asked questions about Ilumya.
Are there reviews or complaints available from people who’ve used Ilumya?
The manufacturer of the drug has testimonials available from people who’ve used Ilumya.
Keep in mind that your results from treatment with a drug may differ from other people’s results. Talk with your doctor to learn more about Ilumya, including whether it may be a good treatment option for you.
How does Ilumya work?
How a drug works is referred to as its mechanism of action.
Ilumya works by blocking the actions of a certain protein in your body. This protein plays a role in your immune system, including increasing inflammation (swelling). By blocking this protein, Ilumya decreases inflammation throughout your body.
If you’d like to learn more about how Ilumya works, talk with your doctor or pharmacist.
Is Ilumya used for psoriatic arthritis?
Ilumya isn’t approved to treat psoriatic arthritis, but the drug may be used off-label for this condition. (Off-label drug use is when an approved drug is prescribed for a purpose other than what it’s approved for.)
If you’d like to learn more about off-label uses of Ilumya, including psoriatic arthritis, talk with your doctor.
When did Ilumya receive FDA approval?
The Food and Drug Administration (FDA) approves new drugs for use, including Ilumya. The drug’s approval date (also called its launch date) was in 2018.
Ilumya is used to treat moderate to severe plaque psoriasis. Ilumya may be prescribed for adults with plaque psoriasis who would benefit from phototherapy (treatment with light) or systemic therapy (treatment that lowers inflammation throughout your body).
Plaque psoriasis is a chronic (long-term) autoimmune condition. (With an autoimmune condition, your immune system attacks your cells by mistake). Plaque psoriasis causes patches of thick, scaly skin. These plaques are often itchy and may be painful.
Plaque psoriasis patches most commonly affect the elbows, knees, lower back, and scalp. But they can appear on other parts of your body as well. Your doctor can determine how severe your plaque psoriasis is by how much of your body these plaques affect.
Ilumya works by blocking the actions of a certain protein in your body. This protein plays a role in your immune system, including increasing inflammation (swelling). By blocking this protein, Ilumya decreases inflammation throughout your body.
If you have questions about how Ilumya is used for plaque psoriasis, talk with your doctor or pharmacist.
Other uses of Ilumya
Ilumya may also be used off-label for other conditions. (Off-label drug use is when an approved drug is prescribed for a purpose other than what it’s approved for.) To learn more, talk with your doctor.
Ilumya and Tremfya are prescription medications that treat moderate to severe plaque psoriasis in adults.
In addition, Tremfya is also used to treat psoriatic arthritis in adults.
Both Ilumya and Tremfya come as a liquid solution inside prefilled syringes. Both drugs are given as an injection under the skin at a doctor’s office or another healthcare facility. Tremfya is also available as a device called the One-Press injector.
To learn more about how Ilumya and Tremfya are alike and different, see this side-by-side comparison. You can also talk with your doctor or pharmacist to see if one of these drugs may be right for you.
Your doctor will explain how you’ll receive Ilumya. They will also explain how much you’ll receive and how often.
Receiving Ilumya
Ilumya comes as a liquid solution inside prefilled syringes. You’ll receive Ilumya as an injection under your skin at your doctor’s office or another healthcare facility. Your doctor will choose an area with clear skin that is not tender or bruised. They may give the injection into your:
- belly, at least 2 inches from your belly button
- upper arm
- thigh
Questions for your doctorYou may have questions about Ilumya and your treatment plan. It’s important to discuss all your concerns with your doctor.
Here are a few tips that might help guide your discussion:
- Before your appointment, write down questions such as:
- How will Ilumya affect my body, mood, or lifestyle?
- Bring someone with you to your appointment if doing so will help you feel more comfortable.
- If you don’t understand something related to your condition or treatment, ask your doctor to explain it to you.
Remember, your doctor and other healthcare professionals are available to help you. And they want you to get the best care possible. So, don’t be afraid to ask questions or offer feedback on your treatment.
Some important things to discuss with your doctor when considering Ilumya treatment include your overall health and any medical conditions you may have.
Interactions
Taking a medication with certain vaccines, foods, and other things can affect how the medication works. These effects are called interactions.
Before taking Ilumya, be sure to tell your doctor about all medications you take, including prescription and over-the-counter types. Also, describe any vitamins, herbs, or supplements you use. Your doctor or pharmacist can tell you about any interactions these items may cause with Ilumya.
Interactions with drugs or supplements
There currently aren’t medications or supplements known to interact with Ilumya. But this doesn’t mean drug interactions with Ilumya won’t be recognized in the future. For example, new medications may be approved that interact with Ilumya.
For this reason, you should still tell your doctor and pharmacist about any medications you take besides Ilumya. This way, they can check for any new interactions during your treatment.
Other interactions
You should avoid getting live vaccines while you’re receiving Ilumya.
Live vaccines contain a weakened version of the virus they protect against. Because Ilumya works by weakening your immune system, your body may not be able to fight the weakened virus in the vaccine. And the vaccine may not be effective if you receive it during your Ilumya treatment.
Examples of live vaccines include:
Before beginning treatment with Ilumya, talk with your doctor or pharmacist about any vaccines you may need.
Warnings
Ilumya may not be right for you if you have certain medical conditions or other factors that affect your health. Talk with your doctor about your health history before you take Ilumya. Factors to consider include those in the list below.
- Active infection. Before starting treatment with Ilumya, tell your doctor if you have an active infection. (An active infection means you’re currently experiencing symptoms.) Ilumya works by weakening your immune system. This can make it harder to treat infections while you’re receiving the drug. Your doctor can determine the best treatment for your infection and whether Ilumya is safe for you. They may wait until your infection clears before prescribing Ilumya for you.
- Tuberculosis (TB), including TB infection in the past. Before beginning Ilumya treatment, it’s important to tell your doctor if you have TB or have had it in the past. Ilumya works by weakening your immune system, which can make TB harder to treat. And, if you’ve had TB in the past, having a weakened immune system may cause the infection to become active (cause symptoms) again. Your doctor will test you for TB before prescribing Ilumya for you. If the test shows you do have TB, your doctor may want to treat it first before you begin using Ilumya. They’ll also monitor you for symptoms of TB during and after your Ilumya treatment.
- Allergic reaction. If you’ve had an allergic reaction to Ilumya or any of its ingredients, your doctor will likely not prescribe Ilumya. Ask them what other medications are better options for you.
Ilumya and alcohol
It should be safe to drink alcohol during your Ilumya treatment. But alcohol use can cause diarrhea, which is also a side effect of Ilumya. Drinking alcohol during your treatment could raise your risk of diarrhea or make it worse if you have it.
In addition, some
If you drink alcohol, talk with your doctor about how much may be safe for you to drink with your condition and treatment plan.
Pregnancy and breastfeeding
It’s not known whether it’s safe to use Ilumya during pregnancy or while breastfeeding.
If you’re pregnant or breastfeeding or planning to become pregnant or breastfeed, talk with your doctor before starting treatment with Ilumya.
If you’re considering treatment with Ilumya, talk with your doctor or pharmacist. Ask questions to better understand the benefits and risks of using the drug. Some examples to help you get started are:
- What should I know about alternative treatment options for Ilumya?
- If I experience side effects from Ilumya, can my dose be adjusted?
- How will I know if Ilumya is working for me?
- Are there lab tests I’ll need to have done during my Ilumya treatment?
You can also learn more about plaque psoriasis treatments here or sign up for Healthline’s psoriasis newsletter to learn more about the condition.
Q:
Is it safe to get a COVID-19 vaccine during my Ilumya treatment?
AnonymousA:
According to the National Psoriasis Foundation, receiving a COVID-19 vaccine during treatment with a psoriasis drug such as Ilumya should be safe and effective.
The COVID-19 vaccine won’t weaken your immune system, as it’s not a live vaccine. (Live vaccines contain a weakened version of the virus they protect against.) To learn more about Ilumya and live vaccines, see the “What should be considered before taking Ilumya?” section above.
You should still talk with your doctor before receiving any vaccine, including a COVID-19 vaccine, during your Ilumya treatment. Your doctor can advise you on which vaccines are safe for you to receive.
The Healthline Pharmacist TeamAnswers represent the opinions of our medical experts. All content is strictly informational and should not be considered medical advice.Disclaimer: Healthline has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.