- Fentanyl transdermal patch is available as a generic drug and as a brand-name drug. Brand name: Duragesic.
- Fentanyl also comes as a buccal and sublingual tablet, oral lozenge, sublingual spray, nasal spray, and injectable.
- Fentanyl transdermal patch is used to treat chronic pain in opioid-tolerant people.
Fentanyl is a prescription drug. It comes in the following forms:
- Transdermal patch: a patch that you place on your skin
- Buccal tablet: a tablet that you dissolve between your cheek and gums
- Sublingual tablet: a tablet that you dissolve under your tongue
- Sublingual spray: a solution that you spray under your tongue
- Oral lozenge: a lozenge that you suck on until it dissolves
- Nasal spray: a solution that you spray into your nose
- Injectable: an injectable solution that’s only given by a healthcare provider
Fentanyl transdermal patch is available as the brand-name drug Duragesic. It’s also available as a generic drug. Generic drugs usually cost less than the brand-name version. In some cases, the brand-name drug and the generic version may be available in different forms and strengths.
Fentanyl transdermal patch may be used as part of a combination therapy. This means you may need to use it with other medications.
Why it’s used
Fentanyl transdermal patch is used to treat chronic pain in opioid-tolerant people. These are people who have taken another opioid pain drug that no longer works as well.
How it works
Fentanyl belongs to a class of drugs called opioid agonists. A class of drugs is a group of medications that work in a similar way. These drugs are often used to treat similar conditions.
Fentanyl works in your brain to change how your body feels and responds to pain.
Fentanyl can cause mild or serious side effects. The following list contains some of the key side effects that may occur while taking fentanyl. This list doesn’t include all possible side effects.
For more information on the possible side effects of fentanyl, or tips on how to deal with a troubling side effect, talk with your doctor or pharmacist.
Fentanyl can also cause other side effects.
More common side effects
The more common side effects that can occur with fentanyl include:
- redness and irritation of your skin where you apply the patch
- nausea
- vomiting
- tiredness
- dizziness
- trouble sleeping
- constipation
- increased sweating
- feeling cold
- headache
- diarrhea
- loss of appetite
These effects may go away within a few days or a couple of weeks. If they’re more severe or don’t go away, talk to your doctor or pharmacist.
Serious side effects
Call your doctor right away if you have serious side effects. Call 911 or go to your local emergency room if your symptoms feel life threatening or if you think you’re having a medical emergency.
Serious side effects and their symptoms can include the following:
- Serious breathing problems. Symptoms can include:
- very shallow breathing (little chest movement with breathing)
- fainting, dizziness, or confusion
- Severely low blood pressure. Symptoms can include:
- dizziness or lightheadedness, especially if you stand up too quickly
- Physical addiction, dependence, and withdrawal when stopping the drug. Symptoms can include:
- restlessness
- irritability or anxiousness
- trouble sleeping
- increase in your blood pressure
- fast breathing rate
- fast heart rate
- dilated pupils (the dark centers of your eyes)
- nausea, vomiting, and a loss of appetite
- diarrhea and stomach cramps
- sweating
- chills, or hairs on your arms “stand up”
- muscle aches and backache
- Adrenal insufficiency. Symptoms can include:
- long-lasting tiredness
- muscle weakness
- pain in your abdomen
- Androgen deficiency. Symptoms can include:
- tiredness
- trouble sleeping
- decreased energy
ConstipationConstipation (infrequent or hard bowel movements) is a very common side effect of fentanyl and other opioid medications. It’s unlikely to go away without treatment.
To help prevent or treat constipation while taking fentanyl, talk to your doctor about dietary changes, laxatives (drugs that treat constipation), and stool softeners. A doctor may prescribe laxatives with opioids to help prevent constipation.
Drop in blood pressure with dosage changesAfter your first dose and when your doctor increases your doses of fentanyl, you may have a drop in blood pressure. Your doctor may have you check your blood pressure during these time periods.
The fentanyl dosage your doctor prescribes will depend on several factors. These include:
- the type and severity of the condition you’re using fentanyl to treat
- your age
- the form of fentanyl you take
- other medical conditions you may have
- whether you have used opioids before
- your tolerance levels
Typically, your doctor will start you on a low dosage and adjust it over time to reach the dosage that’s right for you. They’ll ultimately prescribe the smallest dosage that provides the desired effect.
The following information describes dosages that are commonly used or recommended. However, be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosage to suit your needs.
Forms and strengths
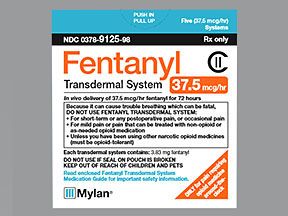
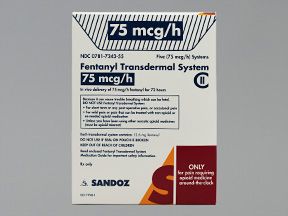
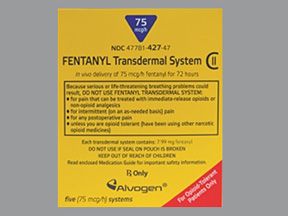
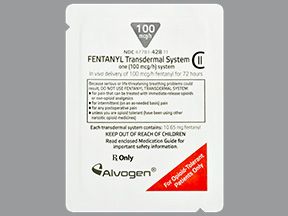
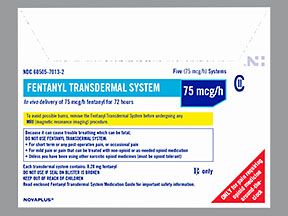
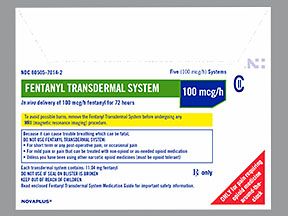
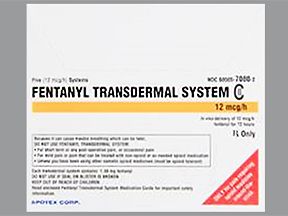
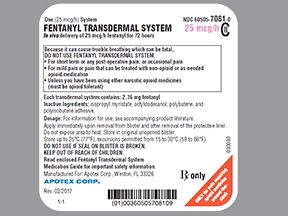
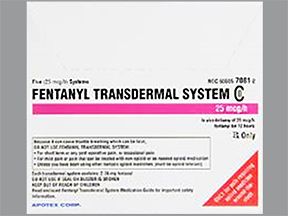
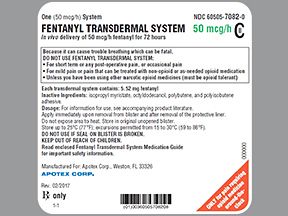
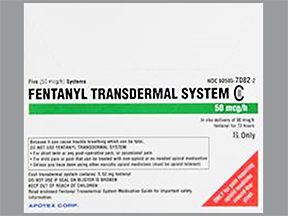
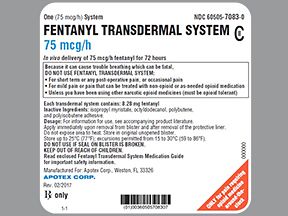
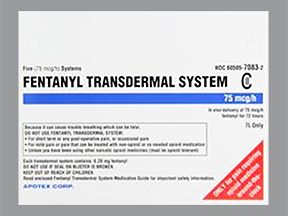
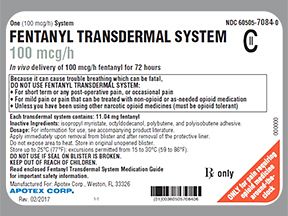
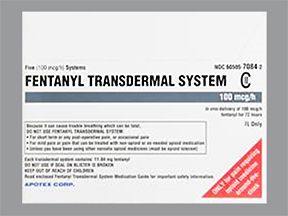
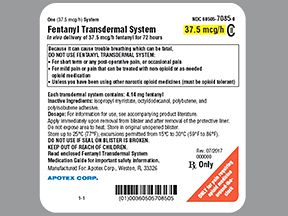
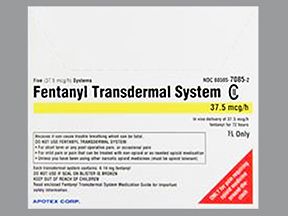
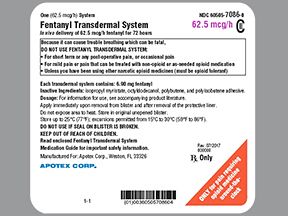
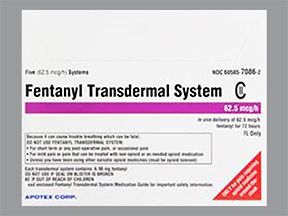
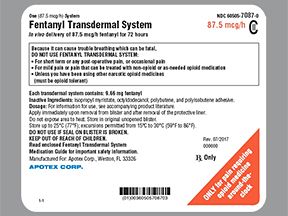
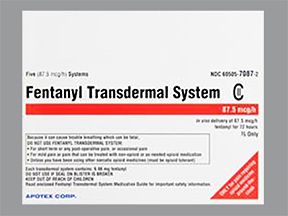
- Generic: fentanyl
- Form: transdermal patch
- Strengths: 12.5 micrograms (mcg)/hour, 25 mcg/hour, 37.5 mcg/hour, 50 mcg/hour, 62.5 mcg/hour, 75 mcg/hour, 87.5 mcg/hour, and 100 mcg/hour
- Brand: Duragesic
- Form: transdermal patch
- Strengths: 12.5 mcg/hour, 25 mcg/hour, 37.5 mcg/hour, 50 mcg/hour, 75 mcg/hour, and 100 mcg/hour
Dosage for severe chronic pain
Adult dosage (ages 18–64 years)
- Your doctor will base your starting dosage on the type of drug and dosage you currently take to control pain. Your doctor will prescribe the least amount of fentanyl to control your pain, with the least amount of side effects.
- Your doctor may increase your dosage based on your level of pain. Your dosage won’t be increased sooner than 3 days after you take your first dose. After that, your doctor may increase your dosage every 6 days as needed.
- Your doctor will regularly check to see if you still need to keep using this drug.
- You should change your patch every 72 hours.
Child dosage (ages 2–17 years)
- Your doctor will base your child’s starting dosage on the type of drug and dosage your child currently takes to control pain. Your doctor will prescribe the least amount of fentanyl to control your child’s pain, with the least amount of side effects.
- Your doctor may increase your child’s dosage based on your child’s level of pain. The dosage won’t be increased sooner than 3 days after your child takes the first dose. After that, your doctor may increase the dosage every 6 days as needed.
- Your doctor will regularly check to see if your child still needs to keep using this drug.
- You should change your child’s patch every 72 hours.
Child dosage (ages 0–1 years)
Fentanyl transdermal patch hasn’t been established as safe or effective for use in children younger than 2 years.
Senior dosage (ages 65 years and older)
The kidneys of older adults may not work as well as they used to. This can cause your body to process drugs more slowly. As a result, more of a drug stays in your body for a longer time. This increases your risk of side effects.
Your doctor may start you on a lowered dosage or a different dosing schedule. This can help keep levels of this drug from building up too much in your body.
Special dosage considerations
- For people with liver disease: Your doctor may start with half the usual dose or avoid use, depending on how severe your disease is.
- For people with kidney disease: Your doctor should start with half the usual dose or avoid use, depending on how severe your disease is.
Fentanyl transdermal patch is generally used for long-term treatment of severe chronic pain. It comes with serious risks if you don’t take it as prescribed.
If you stop taking the drug or don’t take it at all: If you don’t take it at all, you’ll continue to experience pain. If you stop taking the drug suddenly, you may experience symptoms of withdrawal, which can include:
- restlessness
- irritability or anxiousness
- trouble sleeping
- increase in your blood pressure
- fast breathing rate
- fast heart rate
- dilated pupils of your eyes
- nausea, vomiting, and a loss of appetite
- diarrhea and stomach cramps
- sweating
- chills or hairs on your arms “stand up”
- muscle aches and backache
If you miss doses or don’t take the drug on schedule: Your medication may not work as well or may stop working completely. For this drug to work well, a certain amount needs to be in your body at all times.
If you take too much: You could have dangerous levels of the drug in your body. Symptoms of an overdose of this drug can include:
- slowed breathing or changes in normal breathing pattern
- trouble speaking
- confusion
- irritability
- extreme tiredness and drowsiness
- cold and clammy skin
- skin color turning blue
- muscle weakness
- pinpoint pupils
- slow heart rate
- dangerous heart problems
- low blood pressure
- coma
If you think you’ve taken too much of this drug, call your doctor or seek guidance from the American Association of Poison Control Centers at 800-222-1222 or through their online tool. But if your symptoms are severe, call 911 or go to the nearest emergency room right away.
What to do if you miss a dose: Apply your new patch as soon as you remember. Never try to catch up by taking two doses at once. This could result in dangerous side effects.
How to tell if the drug is working: You should feel less pain.
This drug comes with various warnings.
FDA warnings
- This drug has boxed warnings. These are the most serious warnings from the Food and Drug Administration (FDA). A boxed warning alerts doctors and patients about drug effects that may be dangerous.
- Addiction and misuse warning. This drug can lead to addiction and misuse, which can result in overdose and death. Your doctor will assess your risk for addiction and misuse before and during treatment with the fentanyl transdermal patch.
- Decreased breathing rate warning. Fentanyl can make you breathe more slowly. This can lead to breathing failure and possibly death. Your risk is higher if you are older, have lung disease, or are given large initial doses. It’s also higher if you use fentanyl with other medications that can affect your breathing pattern.
- Heat exposure warning. Once you have applied the fentanyl patch to your skin, avoid exposing it to heat. This can cause your body to absorb more fentanyl than you should. This could result in a drug overdose and even death.
- Opioid withdrawal in newborns warning. If a woman takes this drug for a long time during pregnancy, it can lead to opioid withdrawal syndrome in a newborn. This can be life threatening for the baby. Symptoms of withdrawal may include irritability, hyperactivity and unusual sleep pattern, and high-pitched cry. They can also include tremor, vomiting, diarrhea, and failure to gain weight.
Allergy warning
Fentanyl can cause a severe allergic reaction. Symptoms can include:
- rash
- swelling of your face
- throat tightness
- trouble breathing
If you have an allergic reaction, call your doctor or local poison control center right away. If your symptoms are severe, call 911 or go to the nearest emergency room.
Don’t take this drug again if you’ve ever had an allergic reaction to it. Taking it again could be fatal (cause death).
Alcohol interaction warning
The use of drinks that contain alcohol can increase your risk of serious side effects from fentanyl. It may even result in coma or death. You should not drink alcohol while taking fentanyl.
Warnings for people with certain health conditions
For people with breathing problems: Fentanyl may decrease your breathing rate. Use this medication with extreme caution if you’ve been diagnosed with a breathing problem, such as chronic obstructive pulmonary disease (COPD). Do not use fentanyl if you have asthma.
For people with intestinal blockage and constipation: Fentanyl can make these conditions worse. Do not use fentanyl if you have these conditions.
For people with head injury or seizures: Fentanyl may cause increased pressure in your brain and cause breathing problems.
For people with liver disease: Your body may process drugs more slowly. As a result, more of a drug stays in your body for a longer time. This increases your risk of side effects. Your doctor may start you on a lower dosage. This can help keep levels of this drug from building up too much in your body.
For people with kidney disease: If you have kidney disease or a history of kidney disease, you may not be able to clear this drug from your body well. This may increase the levels of fentanyl in your body and cause more side effects.
For people with adrenal insufficiency: Taking this drug can reduce the amount of hormones your adrenal glands release. If you have adrenal insufficiency, taking this drug can make it worse.
For people with pancreas and gallbladder problems: Taking this drug can cause spasms that can make symptoms of conditions such as biliary tract disease and pancreatitis worse.
For people with urination problems: Taking this drug can cause your body to retain urine. If you already have trouble urinating, your doctor may prescribe a lower dosage.
For people with slow heart rate: Taking this drug can slow your heart rate. If you already have a slow heart rate (bradycardia), this drug can make it worse. Use fentanyl with caution. Your doctor may prescribe a lower dosage and monitor you more closely for side effects.
Warnings for other groups
For pregnant women: There haven’t been enough studies done in humans to show if fentanyl poses a risk to a human fetus. Research in animals has shown dangerous effects to the fetus when the mother takes the drug. However, animal studies don’t always predict the way humans would respond.
If a woman takes this drug for a long time during pregnancy, it can lead to opioid withdrawal syndrome in a newborn. This can be life threatening for the baby. Symptoms of withdrawal may include irritability, hyperactivity and unusual sleep pattern, and high-pitched cry. They can also include tremor, vomiting, diarrhea, and failure to gain weight.
For women who are breastfeeding: Fentanyl passes into breast milk and may cause side effects in a child who is breastfed. Talk to your doctor if you breastfeed your child. You may need to decide whether to stop breastfeeding or stop taking this drug.
For seniors: The kidneys of older adults may not work as well as they used to. This can cause your body to process drugs more slowly. As a result, more of a drug stays in your body for a longer time. This increases your risk of side effects.
For children: Fentanyl transdermal patch has not been established as safe or effective for use in children younger than 2 years.
Fentanyl can interact with several other medications. Different interactions can cause different effects. For instance, some can interfere with how well a drug works, while others can cause increased side effects.
Below is a list of medications that can interact with fentanyl. This list doesn’t contain all drugs that may interact with fentanyl.
Before taking fentanyl, be sure to tell your doctor and pharmacist about all prescription, over-the-counter, and other drugs you take. Also tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you avoid potential interactions.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
Drugs you should not take with fentanyl
Do not take these drugs with fentanyl. Taking fentanyl with these drugs can cause dangerous effects in your body. Examples of these drugs include:
- Buprenorphine.
- Taking this drug with fentanyl may lower the effect of fentanyl, cause withdrawal symptoms, or both.
- Depression drugs such as monoamine oxidase inhibitors (MAOIs).
- Taking these drugs with fentanyl may cause anxiety, confusion, slowed breathing, or coma. Do not take fentanyl if you’re taking MAOIs or have taken MAOIs within the last 14 days.
Interactions that increase the risk of side effects
Taking fentanyl with certain medications may result in an increase in negative effects. Examples of these drugs include:
- Muscle relaxants, such as baclofen, cyclobenzaprine, and methocarbamol.
- You may experience increased breathing problems.
- Hypnotics, such as zolpidem, temazepam, and estazolam.
- You may experience increased breathing problems, low blood pressure, extreme drowsiness, or coma. Your doctor may prescribe a lower dosage for you.
- Anticholinergic drugs, such as atropine, scopolamine, and benztropine.
- You may experience increased problems urinating or severe constipation, which could lead to more serious bowel problems.
- Voriconazole and ketoconazole.
- These drugs may increase fentanyl levels in your body, which may increase your risk of side effects. Your doctor may monitor you more frequently and adjust your dosage as needed.
- Erythromycin.
- This medication may increase fentanyl levels in your body, which may increase your risk of side effects. Your doctor may monitor you more frequently and adjust your dosage as needed.
- Ritonavir.
- This medication may increase fentanyl levels in your body, which may increase your risk of side effects. Your doctor may monitor you more frequently and adjust your dosage as needed.
Interactions that can make drugs less effective
When fentanyl is used with certain drugs, it may not work as well to treat your condition. Examples of these drugs include:
- Rifampin.
- This drug may decrease fentanyl levels in your body, making the fentanyl less effective in relieving your pain. Your doctor may monitor you more often and adjust your dosage as needed.
- Carbamazepine, phenobarbital, and phenytoin.
- These drugs may decrease fentanyl levels in your body, making the fentanyl less effective in relieving your pain. Your doctor may monitor you more often and adjust your dosage as needed.
Keep these considerations in mind if your doctor prescribes fentanyl transdermal patch for you.
Storage
- Store this drug at room temperature between 68°F and 77°F (20°C and 25°C).
- Keep this drug in the original unopened pouch.
- Don’t store this medication in moist or damp areas, such as bathrooms.
- Protect fentanyl from theft. Keep it in a locked cabinet or drawer.
Disposal
Take care when disposing of fentanyl patches. When you finish with a patch, do the following:
- Fold the patch so that the adhesive sticks to itself.
- Flush the folded patch down the toilet.
Refills
A prescription for this medication isn’t refillable. You or your pharmacy will have to contact your doctor for a new prescription if you need this medication refilled.
Travel
When traveling with your medication:
- Always carry your medication with you. When flying, never put it into a checked bag. Keep it in your carry-on bag.
- Don’t worry about airport X-ray machines. They can’t hurt your medication.
- You may need to show airport staff the pharmacy label for your medication. Always carry the original prescription-labeled box with you.
- Don’t put this medication in your car’s glove compartment or leave it in the car. Be sure to avoid doing this when the weather is very hot or very cold.
Self-management
- Talk to your doctor or pharmacist on how to properly apply and handle the fentanyl patch. Serious side effects, including death, can occur if you’re exposed to too much of this drug.
- Avoid certain activities that will increase your body temperature while using the fentanyl patch. This increase in temperature can cause an overdose of fentanyl that can lead to death. Examples of activities you should avoid include the following:
- Don’t take hot baths.
- Don’t sunbathe.
- Don’t use hot tubs, saunas, heating pads, electric blankets, heated waterbeds, or tanning lamps.
- Don’t engage in exercise that increases your body temperature.
Clinical monitoring
You doctor should monitor you while you take this drug. Things your doctor will check include:
- Your breathing rate. Your doctor will monitor for any changes in your breathing pattern, especially when you first start taking this drug and after any dose increases.
- Your blood pressure. Your doctor should check your blood pressure regularly.
- Your liver and kidney function. Your doctor may have blood tests done to see how well your kidneys and liver are working. If your kidneys and liver aren’t working well, your doctor may decide to lower your dose of this drug.
- Whether you have signs of addiction. Your doctor will monitor you for signs of addiction while you take this drug.
Diet considerations
Don’t eat grapefruit or drink grapefruit juice while taking fentanyl. This may lead to dangerously high levels of fentanyl in your body.
Availability
Not every dosage form and strength of this drug may be available. When filling your prescription, be sure to call your pharmacy to make sure it has the exact form and strength your doctor prescribed.
Prior authorization
Many insurance companies require a prior authorization for this drug. This means your doctor will need to get approval from your insurance company before your insurance company will pay for the prescription.
There are other drugs available to treat your condition. Some may be better suited for you than others. Talk to your doctor about other drug options that may work for you.
Disclaimer: Healthline has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or other healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.