Highlights for theophylline
- Theophylline oral tablet is only available as a generic drug.
- Theophylline is used to treat the symptoms of asthma or other lung conditions that block your airways, such as emphysema or chronic bronchitis. It’s used for long-term treatment.
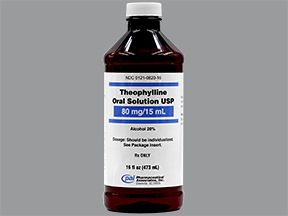
- This drug comes in the form of an oral tablet, oral capsule, or oral solution. You take these drugs by mouth.
- Nausea and vomiting: If you have these symptoms while taking this drug, you may have too much theophylline in your body. Your doctor may check the amount of this drug in your body.
- Smoking: Smoking cigarettes or marijuana can affect the amount of theophylline in your body. Tell your doctor if you smoke.
Theophylline is a prescription drug. It’s available as an oral solution, an extended-release tablet, and an extended-release capsule. It’s also available in an intravenous (IV) form, which is only given by a healthcare provider.
The theophylline tablet is only available as a generic drug. Generic drugs usually cost less than the brand-name version.
Why it’s used
Theophylline is used to treat the symptoms of asthma or other lung conditions that block your airways, such as emphysema or chronic bronchitis.
Theophylline may be used as part of a combination therapy. This means you may need to take it with other medications.
How it works
Theophylline belongs to a class of drugs called methylxanthines. A class of drugs is a group of medications that work in a similar way. These drugs are often used to treat similar conditions.
Theophylline works by opening the airways in your lungs. It does this by relaxing the muscles and decreasing the response to substances that cause your airways to constrict. This makes it easier for you to breathe.
Theophylline oral tablet doesn’t cause drowsiness but it can cause other side effects.
More common side effects
Some of the more common side effects that can occur with use of theophylline include:
- headache
- trouble sleeping
If these effects are mild, they may go away within a few days or a couple of weeks. If they’re more severe or don’t go away, talk to your doctor or pharmacist.
Serious side effects
Call your doctor right away if you have serious side effects. Call 911 if your symptoms feel life threatening or if you think you’re having a medical emergency. Serious side effects and their symptoms can include the following:
- Irregular heart rate. Symptoms can include:
- shortness of breath
- dizziness
- fluttering or pain in your chest
- Seizure. Symptoms can include:
- confusion
- trouble talking
- tremors or twitching
- loss of muscle tone or tense muscles
Disclaimer: Our goal is to provide you with the most relevant and current information. However, because drugs affect each person differently, we cannot guarantee that this information includes all possible side effects. This information is not a substitute for medical advice. Always discuss possible side effects with a healthcare provider who knows your medical history.
Theophylline oral tablet can interact with other medications, vitamins, or herbs you may be taking. An interaction is when a substance changes the way a drug works. This can be harmful or prevent the drug from working well.
To help avoid interactions, your doctor should manage all of your medications carefully. Be sure to tell your doctor about all medications, vitamins, or herbs you’re taking. To find out how this drug might interact with something else you’re taking, talk to your doctor or pharmacist.
Examples of drugs that can cause interactions with theophylline are listed below.
Alcohol abuse drugs
These drugs can increase the levels of theophylline in your body. This means that you may have more side effects. An example of these drugs is:
- disulfiram
Anxiety drugs
When you take these drugs with theophylline, you may need a larger dose for them to work. Examples of these drugs include:
- diazepam
- flurazepam
- lorazepam
- midazolam
Blood clot drugs
These drugs may increase the levels of theophylline in your body. This means that you may have more side effects. Examples of these drugs include:
- pentoxifylline
- ticlopidine
Depression drugs
These drugs may increase the levels of theophylline in your body. This means that you may have more side effects. An example of these drugs is:
- fluvoxamine
Gout drugs
These drugs may increase the levels of theophylline in your body. This means that you may have more side effects. An example of these drugs is:
- allopurinol
Heart rhythm drugs
These drugs may increase the levels of theophylline in your body. This means that you may have more side effects. Examples of these drugs include:
- mexiletine
- propafenone
- verapamil
- propranolol
Hepatitis drugs
These drugs may increase the levels of theophylline in your body. This means that you may have more side effects. An example of these drugs is:
- interferon alfa-2a
Hormone problems/birth control drugs
These drugs may increase the levels of theophylline in your body. This means that you may have more side effects. An example of these drugs is:
- estrogen
Immune disorder drugs
These drugs may increase the levels of theophylline in your body. This means that you may have more side effects. An example of these drugs is:
- methotrexate
Infection drugs
These drugs may increase the levels of theophylline in your body. This means that you may have more side effects. Examples of these drugs include:
- ciprofloxacin
- clarithromycin
- erythromycin
Ketamine
This drug raises your risk of side effects from theophylline.
Lithium
When taken with theophylline, you may need a larger dose of lithium for it to work.
Seizure drugs
These drugs may decrease the levels of theophylline in your body. This means that it may not work to treat your condition. Examples of these drugs include:
- phenobarbital
- phenytoin
Stomach acid drugs
These drugs may increase the levels of theophylline in your body. This means that you may have more side effects. An example of these drugs is:
- cimetidine
Other drugs
These drugs may decrease the levels of theophylline in your body. This means that it may not work to treat your condition. Examples of these drugs include:
- carbamazepine
- rifampin
- St. John’s wort
Disclaimer: Our goal is to provide you with the most relevant and current information. However, because drugs interact differently in each person, we cannot guarantee that this information includes all possible interactions. This information is not a substitute for medical advice. Always speak with your healthcare provider about possible interactions with all prescription drugs, vitamins, herbs and supplements, and over-the-counter drugs that you are taking.
This drug comes with several warnings.
Alcohol warning
The use of drinks that contain alcohol raises your risk of side effects from theophylline. If you drink alcohol, talk to your doctor.
Warnings for people with certain health problems
For people with liver disease: You may not be able to clear theophylline from your body well. This may increase the amount of this drug in your body and cause more side effects.
For people with heart failure: You may not be able to clear theophylline from your body well. This may increase the amount of this drug in your body and cause more side effects.
For people with ulcers: This drug may make your ulcers worse.
For people with seizures: This drug may make your seizures worse.
For people with an irregular heart rate: This drug may make your irregular heart rate worse.
For people with low thyroid levels: You may not be able to clear theophylline from your body well. This may increase the amount of this drug in your body and cause more side effects.
Warnings for certain groups
For pregnant women: Theophylline is a category C pregnancy drug. That means two things:
- Research in animals has shown adverse effects to the fetus when the mother takes the drug.
- There haven’t been enough studies done in humans to be certain how the drug might affect the fetus.
Talk to your doctor if you’re pregnant or planning to become pregnant. This drug should be used only if the potential benefit justifies the potential risk to the fetus.
For women who are breastfeeding: Theophylline may pass into breast milk and may cause side effects in a child who is breastfed. Talk to your doctor if you breastfeed your child. You may need to decide whether to stop breastfeeding or stop taking this medication.
For seniors: Theophylline is cleared from the body more slowly in adults over the age of 60 years. Your doctor may monitor you more closely for side effects. The amount of theophylline in your blood may also be monitored more closely.
For children: Theophylline is safe for children. However, theophylline is removed more slowly from the body in children under 1 year old. Your doctor should monitor your infant carefully if they take this drug.
All possible dosages and forms may not be included here. Your dose, form, and how often you take it will depend on:
- your age
- the condition being treated
- how severe your condition is
- other medical conditions you have
- how you react to the first dose
Forms and strengths
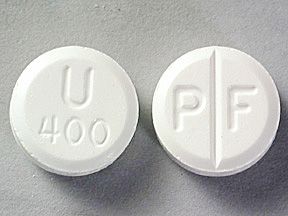
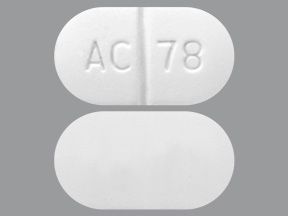
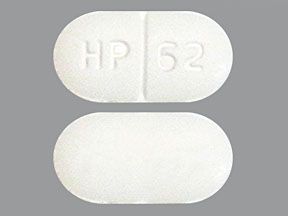
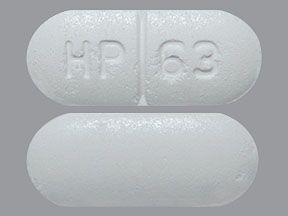
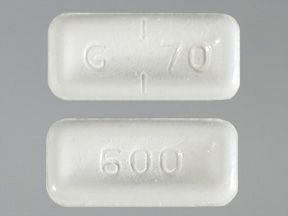
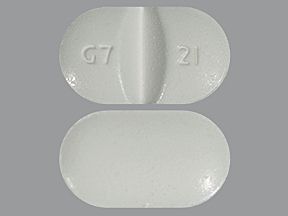
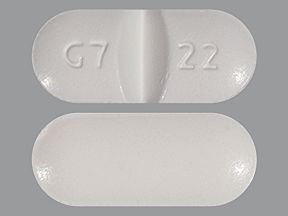
Generic: Theophylline
- Form: extended-release tablet
- Strengths: 100 mg, 200 mg, 300 mg, 400 mg, 450 mg, 600 mg
Dosage for asthma or other lung diseases
Adult dosage (ages 18–59 years)
The usual starting dose is 300–400 mg per day. After 3 days, your dose may be increased to 400–600 mg per day if you don’t have any side effects. After 3 more days, if your dose is tolerated and more medication is needed, your dose may be adjusted based on the level of theophylline in your blood.
Child dosage (ages 16–17 years)
The usual starting dose is 300–400 mg per day. After 3 days, your dose may be increased to 400–600 mg per day if you don’t have any side effects. After 3 more days, if your dose is tolerated and more medication is needed, your dose may be adjusted based on the level of theophylline in your blood.
Child dosage (ages 1–15 years who weigh more than 45 kg)
The starting dose is 300–400 mg per day. After 3 days, your doctor may increase your dose to 400–600 mg per day. After 3 more days, your dose may be adjusted as needed based on the level of theophylline in your blood.
Child dosage (ages 1–15 years who weigh less than 45 kg)
The starting dose is 12–14 mg/kg per day up to 300 mg per day. After 3 days, your doctor may increase your dose to 16 mg/kg daily up to a maximum of 400 mg per day if you don’t have any side effects. After 3 more days, if the dose is tolerated, it may be increased to 20 mg/kg daily up to a maximum of 600 mg per day.
This drug is given in divided doses every 4–6 hours. Your dose will be adjusted based on the amount of theophylline in the blood.
Child dosage (babies born at full-term up to 12 months of age)
Your doctor will calculate your child’s dose based on their age and body weight. The dose will be adjusted based on the amount of theophylline in the blood.
- For infants 0–25 weeks: The total daily dose should be divided into 3 equal doses taken by mouth every 8 hours.
- For infants 26 weeks of age and older: The total daily dose should be divided into 4 equal doses taken by mouth every 6 hours.
Child dosage (babies born prematurely less than 12 months old)
- Babies younger than 24 days: 1 mg/kg of body weight
- Babies 24 days and older: 1.5 mg/kg of body weight
Senior dosage (ages 60 years and older)
- The kidneys of older adults may not work as well as they used to. This can cause your body to process drugs more slowly. As a result, more of a drug stays in your body for a longer time. This increases your risk of side effects.
- Your doctor may start you on a lowered dose or a different medication schedule. This can help keep levels of this drug from building up too much in your body.
- Your maximum dose per day shouldn’t be higher than 400 mg.
Special dosage considerations
If you have risk factors for reduced clearance, such as liver disease: Your maximum dose per day shouldn’t be higher than 400 mg.
Disclaimer: Our goal is to provide you with the most relevant and current information. However, because drugs affect each person differently, we cannot guarantee that this list includes all possible dosages. This information is not a substitute for medical advice. Always speak with your doctor or pharmacist about dosages that are right for you.
Theophylline is used for long-term treatment. It comes with risks if you don’t take it as prescribed.
If you stop taking the drug or don’t take it at all
Your symptoms, including trouble breathing, may get worse. This can be fatal (cause death).
If you miss doses or don’t take the drug on schedule
Your medication may not work as well or may stop working completely. For this drug to work well, a certain amount needs to be in your body at all times.
If you take too much
You could have dangerous levels of the drug in your body. You may have the following symptoms:
- severe vomiting
- nausea
- feeling restless or irritated
- seizures
- heart rhythm problems
If you think you’ve taken too much of this drug, call your doctor or local poison control center. If your symptoms are severe, call 911 or go to the nearest emergency room right away.
What to do if you miss a dose
Take the next dose at the usually scheduled time. Don’t make up the missed dose.
How to tell if the drug is working
You may be able to breathe better.
Keep these considerations in mind if your doctor prescribes theophylline for you.
General
- Take the tablets with food. However, don’t take them with a high-fat meal. Taking your dose too close to a high-fat meal may increase your theophylline levels and cause side effects.
- You can cut the scored tablets only.
Storage
- Store theophylline at room temperature between 59°F and 86°F (15°C and 30°C).
- Keep it away from high temperatures.
Refills
A prescription for this medication is refillable. You should not need a new prescription for this medication to be refilled. Your doctor will write the number of refills authorized on your prescription.
Travel
When traveling with your medication:
- Always carry your medication with you. When flying, never put it into a checked bag. Keep it in your carry-on bag.
- Don’t worry about airport X-ray machines. They can’t hurt your medication.
- You may need to show airport staff the pharmacy label for your medication. Always carry the original prescription-labeled box with you.
- Don’t put this medication in your car’s glove compartment or leave it in the car. Be sure to avoid doing this when the weather is very hot or very cold.
Self-management
Your doctor may have you monitor your lung function using a peak flow meter. They will show you how to do this. They may ask you to record your symptoms.
Clinical monitoring
Your doctor may monitor certain health issues. This can help make sure you stay safe while you take this drug. These issues may include:
- Theophylline blood levels. This will help your doctor decide if you’re taking the right dose. Your doctor will monitor these levels as needed. The results will determine if you need a higher or lower dose.
There are other drugs available to treat your condition. Some may be better suited for you than others. Talk to your doctor about other drug options that may work for you.
Disclaimer: Healthline has made every effort to make certain that all information is factually correct, comprehensive, and up-to-date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or other healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.