If you have a certain type of cancer, your doctor may discuss imatinib oral tablets with you.
This is a prescription drug that’s used to treat some types of blood cancer and skin cancer. Specifically, it’s used for certain forms of:
- acute lymphocytic leukemia (ALL) in adults and children
- chronic myeloid leukemia (CML) in adults and children
- systemic mastocytosis (a condition in which you have too many immune cells, called mast cells, in your body) in adults
- myelodysplastic syndromes (a type of cancer that affects your body’s ability to make healthy blood cells) in adults
- hypereosinophilic syndrome (a condition in which you have a high level of blood cells called eosinophils) in adults
- chronic (long-lasting) eosinophilic leukemia (type of blood cancer related to a high level of eosinophils) in adults
- dermatofibrosarcoma protuberans (a type of skin cancer) in adults
To learn more about these cancers, see the “What are imatinib oral tablets used for?” section below.
Imatinib oral tablet basics
Imatinib is an active drug that’s available as a generic medication. It belongs to a group of drugs called tyrosine kinase inhibitors.
This medication comes as oral tablets that you’ll swallow.
In this article, side effects, uses, cost, and more of imatinib oral tablets are described.
Imatinib oral tablet brand-name versions
Imatinib is a generic drug that’s also available as a brand-name drug called Gleevec. To learn more about this brand-name version of imatinib, talk with your doctor.
Imatinib oral tablets are a generic drug, which means they’re an exact copy of the active drug in a brand-name medication. The brand-name medication that imatinib oral tablets are based on is called Gleevec.
Generic drugs are thought to be as safe and effective as the brand-name drug they’re based on. In general, generics usually cost less than brand-name drugs do.
If you’d like to know more about using Gleevec instead of imatinib oral tablets, talk with your doctor. View this Healthline article to learn more about the differences between generic and brand-name drugs.
Like most drugs, imatinib oral tablets may cause mild or serious side effects. The lists below describe some of the more common side effects that imatinib oral tablets may cause. These lists don’t include all possible side effects.
Keep in mind that side effects of a drug can depend on:
- your age
- other health conditions you have
- other medications you may be taking
Your doctor or pharmacist can tell you more about the potential side effects of imatinib oral tablets. They can also suggest ways to help reduce side effects.
Mild side effects
Here’s a short list of some of the mild side effects that imatinib oral tablets can cause. To learn about other mild side effects, talk with your doctor or pharmacist, or read imatinib oral tablets’ prescribing information.
Mild side effects of imatinib oral tablets that have been reported include:
- diarrhea
- edema (swelling) in the ankles, arms, legs, face, or other areas
- nausea and vomiting
- muscle cramps and pain
- joint pain
- fatigue (lack of energy)
- indigestion (upset stomach)
- headache
- common cold, which may lead to cough
- dizziness
- blurred vision
- belly pain
- hair loss*
- rash*
Mild side effects of many drugs may go away within a few days or a couple of weeks. But if they become bothersome, talk with your doctor or pharmacist.
* For more information about this side effect, see the “Side effect focus” section below.
Serious side effects
Serious side effects from imatinib oral tablets can occur, but they aren’t common. If you have serious side effects from imatinib oral tablets, call your doctor right away. But if you think you’re having a medical emergency, you should call 911 or your local emergency number.
Serious side effects of imatinib oral tablets that have been reported include:
- severe fluid buildup around the lungs and heart and in the belly
- severe rash, including those of Stevens-Johnson syndrome and erythema multiforme
- hemorrhage (serious bleeding)
- blood cell problems, such as anemia (low level of red blood cells), thrombocytopenia (low level of platelets), and neutropenia (low level of certain white blood cells)
- gastrointestinal problems, including tears or holes in the stomach or intestines
- liver problems, such as liver damage or liver failure
- hypothyroidism (a condition in which the body doesn’t make enough thyroid hormones)
- heart problems, such as congestive heart failure and left-sided heart failure
- problems with typical growth in children and adolescents
- tumor lysis syndrome (a condition that happens when cancer cells release harmful substances into the blood)
- kidney problems, such as kidney damage
- problems affecting the ability to drive or operate machinery, such as sleepiness, dizziness, or blurry vision
- eye-related side effects,* such as swelling around the eyes or eyelids and other eye problems
- allergic reaction*
* For more information about this side effect, see the “Side effect focus” section below.
Side effect focus
Learn more about some of the side effects imatinib oral tablets may cause.
Eye-related side effects
You may have certain eye issues while you’re taking imatinib oral tablets.
For instance, the drug can cause periorbital edema (swelling around your eyes). In studies, periorbital edema was a common side effect in people taking imatinib.
This drug may also cause blurry vision and some rare eye problems.
Less common eye-related side effects that may happen with imatinib include:
- bleeding in certain areas of the eye, such as the:
- vitreous humor (gel-like substance in the center of your eye)
- retina (thin layer in the back of your eye)
- sclera (white portion of your eye)
- conjunctiva (clear covering over your eye)
- conjunctivitis (pink eye)
- eye dryness, irritation, pain, or swelling
- glaucoma (increased pressure in your eye)
- cataract (cloudiness in the lens of your eye)
What might help
If you have any eye issues or vision changes while you’re taking imatinib, call your doctor.
Depending on how serious your eye problem is, your eye doctor may treat the condition. But in certain cases, your doctor may have you see an eye specialist for serious eye concerns.
If you’re having blurry vision or trouble with your eyesight, don’t drive or do any tasks that require you to see well.
In some cases, your doctor may lower your dose of imatinib or have you stop taking the drug. Ask your doctor what you can do for eye-related side effects with this drug.
Hair loss
In studies, some people who took imatinib had hair loss.
Whether you’ll have hair loss with this drug may depend on individual factors such as:
- your dosage of imatinib, because higher doses may increase the risk of hair loss
- any other medications you’re taking that also have this side effect
- the condition you’re taking imatinib to treat
- other health conditions that cause hair loss, such as hypothyroidism, which is also a side effect of imatinib
What might help
Hair loss is typically a temporary side effect of imatinib. And it resolves once you complete treatment with the drug.
If you’re concerned about hair loss with imatinib, talk with your doctor. They can suggest ways to manage this side effect.
Rash
Imatinib can cause rash and other skin reactions.
Rashes with imatinib can be mild or serious. You may have a greater risk for a rash or skin reaction if you’re taking higher doses of imatinib.
In addition to rash, other skin symptoms that may occur with imatinib include:
- dry skin
- erythema (redness of your skin)
- infected hair follicles
- peeling skin
- purpura (purple-colored spots on your skin)
- skin discoloration, such as a bluish tint
Serious skin reactions that may occur with imatinib include:
- exfoliative dermatitis (a condition that causes peeling skin all over the body)
- Stevens-Johnson syndrome (a condition that causes painful sores on the mouth, eyes, genitals, throat, or over the whole body)
- vesicular rash (a rash with small blisters)
- erythema multiforme (a condition that causes blisters and painful sores)
Keep in mind that an allergic reaction to imatinib may also cause a rash. See the section just below for more details about allergic reaction to this drug.
What might help
If you have a mild rash or skin reaction with imatinib, tell your doctor. They’ll check to make sure the rash isn’t serious.
But if you have a serious rash or skin condition with imatinib, get medical help right away. If your symptoms feel life threatening, call 911 or your local emergency number.
Depending on the severity of your rash, your doctor may suggest that you try an over-the-counter or prescription product to relieve your symptoms. For instance, they may suggest this if you have dry skin or skin irritation.
Allergic reactionSome people may have an allergic reaction to imatinib oral tablets.
Symptoms of a mild allergic reaction can include:
- skin rash
- itchiness
- flushing (temporary warmth, redness, or deepening of skin color)
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include swelling under your skin, typically in your eyelids, lips, hands, or feet. They can also include swelling of your tongue, mouth, or throat, which can cause trouble breathing.
Call your doctor right away if you have an allergic reaction to imatinib oral tablets. But if you think you’re having a medical emergency, call 911 or your local emergency number.
Find answers to some commonly asked questions about imatinib oral tablets.
How does imatinib work? What’s its half-life?
Imatinib belongs to a group of drugs called tyrosine kinase inhibitors. These drugs work by blocking cancer cells from growing. This is imatinib’s mechanism of action (how it works).
Imatinib has a half-life of around 18 hours. A drug’s half-life is the time it takes for your body to clear half of a dose of the drug. Because imatinib’s half-life is 18 hours, it can be taken once each day for most of its uses.
How long imatinib stays in your body depends on:
- other medications you may be taking
- your age
- your overall health
For example, if you have serious liver or kidney problems, it may take longer for imatinib to clear from your body. In that case, the drug would stay in your system for a longer period of time.
Your doctor can provide more information on how this drug works and its half-life.
Is imatinib a chemotherapy drug?
Imatinib isn’t a traditional chemotherapy drug. Instead, it’s a targeted treatment. This means it works by blocking specific targets inside cancer cells.
Chemotherapy, on the other hand, affects all fast-growing cells in your body. It doesn’t target just cancer cells. So chemotherapy affects more cells in your body than targeted therapies do.
Compared with targeted treatments, chemotherapy can make your body more susceptible to infection. It may also cause more serious side effects.
For certain uses, your doctor may prescribe imatinib together with chemotherapy.
Does imatinib treat CLL, AML, or GIST?
Your doctor may prescribe imatinib off-label for these conditions. Off-label use is when a drug is given for a different purpose than its approved uses.
Chronic lymphocytic leukemia (CLL) is a type of cancer that affects white blood cells in your bone marrow. It’s a slow-growing cancer, and its symptoms may not appear for a while. For CLL, your doctor may prescribe imatinib together with other treatments.
Acute myeloid leukemia (AML) is the second most common type of leukemia that affects adults. (Leukemia is cancer of the blood or bone marrow.) AML is a fast-growing, aggressive type of cancer.
In certain cases of AML, doctors may recommend imatinib treatment.
Gastrointestinal stromal tumors (GISTs) are tumors in your gastrointestinal tract. Your doctor may suggest imatinib for treatment because it blocks signals that allow these tumors to grow. It’s important to note that the brand-name version of imatinib, called Gleevec, is approved to treat GIST. But GIST isn’t an approved use for the generic version of imatinib.
If you’d like to know more about using imatinib for any of these conditions, talk with your doctor.
Is imatinib used for breast cancer or melanoma?
Imatinib isn’t approved to treat breast cancer or melanoma (a type of skin cancer).
One 2018
Doctors may recommend using imatinib off-label for melanoma. (Off-label use is when a drug is given for a different purpose than its approved uses.) A 2019
Keep in mind that imatinib is approved to treat dermatofibrosarcoma protuberans, which is a rare type of skin cancer. See the “What are imatinib oral tablets used for?” section below for more information about this. And ask your doctor if you’d like to know more about using imatinib to treat melanoma.
How does imatinib compare with ponatinib?
Ponatinib is the active ingredient of the brand-name drug Iclusig. Imatinib is an active ingredient and a generic version of the brand-name drug Gleevec. Ponatinib isn’t available as a generic medication.
Both imatinib and ponatinib belong to a group of drugs called tyrosine kinase inhibitors. They work in similar ways to treat certain types of leukemia (blood cell cancers).
These medications have some similar uses, side effects, interactions, and warnings. But they have some differences, too.
To learn more about how these two drugs compare, ask your doctor for more information. They can tell you which would be better for you.
If you have a certain type of cancer, your doctor may discuss imatinib oral tablets with you.
This is a prescription drug that’s used to treat types of blood cancer and skin cancer. Specifically, it’s used for certain forms of:
- Acute lymphocytic leukemia (ALL). For ALL, imatinib is used in adults and children ages 1 year and older. ALL is a fast-growing type of cancer that affects the blood or bone marrow. This drug treats:
- ALL in adults that’s Philadelphia chromosome-positive (Ph+) and either refractory or relapsed. Refractory cancer hasn’t improved with past treatments. Relapsed cancer has returned after it reached remission (a phase in which it doesn’t cause symptoms).
- ALL in children that’s been newly diagnosed. For this purpose, imatinib is used together with chemotherapy.
- Chronic myeloid leukemia (CML). For CML, imatinib is used in adults and children ages 1 year and older. CML is a slow-growing type of bone marrow cancer. This drug treats:
- Ph+ CML that’s been newly diagnosed.
- Ph+ CML in three phases: chronic phase, accelerated phase, or blast crisis phase. The chronic phase is the earliest phase of CML. For CML in the chronic phase, imatinib is used after other treatment hasn’t worked. In the accelerated phase, leukemia cells rapidly multiply (make more cells). The blast crisis phase is the most advanced stage of CML.
- Systemic mastocytosis. Systemic mastocytosis is a condition in which you have too many immune cells, called mast cells, in your body. For this use, imatinib is used in adults with an aggressive form of the condition. It’s used for people who don’t have a mutation (abnormal change) in a certain gene or in people whose gene mutation status isn’t known.
- Myelodysplastic syndromes (MDS). MDS is a type of cancer that affects your body’s ability to make healthy blood cells. For this use, imatinib is used in adults. It’s given for MDS that’s related to a change in a certain gene.
- Hypereosinophilic syndrome or chronic (long-lasting) eosinophilic leukemia. Hypereosinophilic syndrome is a condition in which you have a high level of blood cells called eosinophils. And chronic eosinophilic leukemia is a type of blood cancer related to a high level of eosinophils. For these uses, imatinib is used in adults. It can be used in people with one or both of these diseases. It’s given to people with a certain gene mutation. But it can also be used in people who don’t have this mutation or whose gene mutation status isn’t known.
- Dermatofibrosarcoma protuberans. Dermatofibrosarcoma protuberans is a type of skin cancer. For this use, imatinib is used in adults. Imatinib treats this condition when it either can’t be treated with surgery, has returned after past treatment, or is metastatic (has spread to other areas of the body). The drug can be used for cases of dermatofibrosarcoma protuberans that have one or all of these characteristics.
Imatinib is a tyrosine kinase inhibitor. It treats cancer by stopping cancer cells from growing.
Your doctor may also prescribe imatinib off-label for other conditions. Off-label use is when a drug is given for a different purpose than its approved uses.
Costs of prescription drugs can vary depending on many factors. These factors include what your insurance plan covers and which pharmacy you use.
Financial assistance to help you pay for imatinib oral tablets may be available. Medicine Assistance Tool and NeedyMeds are two websites that provide resources to help reduce the cost of imatinib oral tablets.
These websites also offer tools to help you find low-cost healthcare and certain educational resources. To learn more, visit the websites.
Your doctor will explain how you should take imatinib oral tablets. They’ll also explain how much to take and how often. Be sure to follow your doctor’s instructions. Below are commonly used dosages, but always take the dosage your doctor prescribes.
Taking imatinib oral tablets
Imatinib oral tablets are administered orally (taken by mouth). You’ll take them with a meal and a full glass of water.
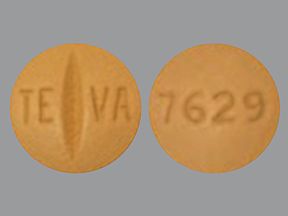
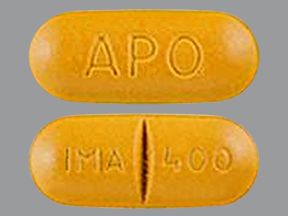
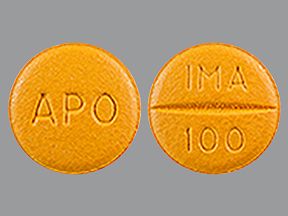
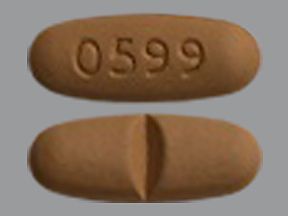
This drug comes in the following strengths:
- 100 milligrams (mg)
- 400 mg
Imatinib oral tablets don’t come in other strengths, such as 200 mg or 300 mg. If you’re prescribed one of these doses, your doctor or pharmacist will tell you how to take it.
Dosage
Your doctor will recommend your imatinib dosage and may adjust it depending on:
- the condition you’re using imatinib to treat and its severity
- other medications you may be taking
- other health conditions you have
- your age
This drug may be taken once a day or twice a day. Your doctor will prescribe the dosage that’s right for your condition.
Taking imatinib oral tablets with other drugs
Your doctor may prescribe imatinib alone or together with other drugs to treat your condition.
For example, in children with acute lymphocytic leukemia, imatinib is used together with chemotherapy.
Your doctor will discuss your treatment plan with imatinib and recommend any other medications you’ll need to take. They may also adjust your dosage of imatinib if you’re taking it with other drugs.
If you’d like, ask your doctor about the pros and cons of using imatinib with other medications.
Questions about taking imatinib oral tablets
Below is a list of common questions related to taking imatinib.
- What if I miss a dose of imatinib oral tablets? If you miss a scheduled dose of imatinib, take it as soon as you remember. But if it’s close to your next scheduled dose, skip the missed dose and continue with your usual schedule. Don’t take two doses of imatinib together. Doing so can increase your risk for serious side effects.
- Will I need to use imatinib oral tablets long term? Imatinib may be used long term if the drug is working for your condition. Your doctor will discuss your treatment plan and recommend how long you’ll likely need to take imatinib. Keep in mind that imatinib doesn’t cure your condition. But, if it’s working to keep you free from symptoms and you don’t have serious side effects, you’ll likely take it long term. While you’re taking this drug, your doctor will order blood tests regularly to see how well it’s working.
- Can imatinib oral tablets be chewed, crushed, or split? No, you should not chew, crush, or split imatinib tablets. If your skin or another body area comes into contact with crushed tablets, wash the area right away with soap and water. Be sure to take imatinib tablets whole, as prescribed. If you have trouble swallowing pills, you can mix the tablet in a glass of water or apple juice. Use about 50 milliliters (mL) of liquid for a 100-mg tablet, or about 200 mL for a 400-mg tablet. Stir the liquid to dissolve the tablet. Once it completely dissolves, drink the mixture. You can also try these tips to help you swallow pills.
- Should I take imatinib oral tablets with food? You should take imatinib tablets with food and a full glass of water. Doing so can help reduce the risk of some side effects of the drug, such as indigestion (upset stomach). But don’t take imatinib with grapefruit or grapefruit juice. Doing this can increase side effects from the drug.
- How long do imatinib oral tablets take to work? This drug starts working soon after you take it. You may start to see some of your symptoms lessen after a few weeks of treatment. Your doctor will order blood tests regularly to see how well imatinib is working for your condition. (But keep in mind, it may take several months for you to be symptom free. And remember that Imatinib doesn’t cure cancer.) Your doctor can tell you more about how long imatinib will take to work for your condition.
Questions for your doctorYou may have questions about imatinib oral tablets and your treatment plan. It’s important to discuss all your concerns with your doctor.
Here are a few tips that might help guide your discussion:
- Before your appointment, write down questions such as:
- How will imatinib oral tablets affect my body, mood, or lifestyle?
- Bring someone with you to your appointment if doing so will help you feel more comfortable.
- If you don’t understand something related to your condition or treatment, ask your doctor to explain it to you.
Remember, your doctor and other healthcare professionals are available to help you. And they want you to get the best care possible. So don’t be afraid to ask questions or offer feedback on your treatment.
Before you begin treatment with imatinib, ask your doctor if this drug is right for you. They’ll discuss your treatment plan, your overall health, and what you can expect with this drug.
Tell your doctor about other medications you’re taking. Also, let them know if you have other health conditions that might affect the treatment of your condition with imatinib.
These and other considerations are described below.
Interactions
Taking medications, vaccines, foods, and other things with a certain drug can affect how the drug works. These effects are called interactions.
Before taking imatinib oral tablets, be sure to tell your doctor about all medications you take, including prescription and over-the-counter types. Also describe any vitamins, herbs, or supplements you use. Your doctor or pharmacist can tell you about any interactions these items may cause with imatinib oral tablets.
Interactions with drugs or supplements
Imatinib oral tablets can interact with several types of drugs. In some cases, interactions can increase side effects of either drug. Interactions may also make medications less effective.
Examples of drugs that may interact with imatinib include:
- the pain reliever and fever reducer acetaminophen (Tylenol)
- certain antibiotics such as rifampin and clarithromycin
- seizure drugs such as phenytoin (Dilantin), carbamazepine (Tegretol), and phenobarbital
- certain antifungal drugs such as itraconazole (Sporanox) and ketoconazole
- certain HIV drugs such as atazanavir, nelfinavir, and ritonavir
- proton pump inhibitors, such as lansoprazole (Prevacid), omeprazole (Prilosec), and esomeprazole (Nexium)
- certain blood pressure medications, such as amlodipine (Norvasc), felodipine, and nifedipine (Procardia, Procardia XL)
- statin drugs such as simvastatin
- benzodiazepines such as lorazepam and diazepam
- certain migraine medications such as ergotamine and dihydroergotamine (DHE-45, Migranal)
- certain pain medications such as alfentanil, fentanyl, oxycodone (Oxycontin, Roxicodone), tramadol (Ultram), and methadone
- heart medications such as pimozide and quinidine
- immunosuppressants such as cyclosporine, everolimus (Afinitor, Zortress), sirolimus (Rapamune), and tacrolimus (Prograf)
- the blood thinner warfarin
- the herb St. John’s wort
This list does not contain all types of drugs that may interact with imatinib oral tablets. Your doctor or pharmacist can tell you more about these interactions and any others that may occur with use of imatinib oral tablets.
Other interactions
In addition to the drugs and supplements listed above, imatinib interacts with grapefruit.
You should avoid drinking grapefruit juice or eating grapefruit with imatinib. Doing so can increase side effects from the drug.
Warnings
Imatinib oral tablets may not be right for you if you have certain medical conditions or other factors that affect your health. Talk with your doctor about your health history before you take imatinib oral tablets. Factors to consider include those in the list below.
- Heart problems. If you have heart problems, imatinib may worsen them. Imatinib can cause fluid buildup, which can damage or weaken your heart. Tell your doctor if you have or have had any heart problems. They can discuss the safety of you using imatinib. If you have hypereosinophilic syndrome, taking imatinib can increase your risk for serious heart damage. (With this syndrome, you have a high level of blood cells called eosinophils.) Your doctor will check your heart function before you start taking imatinib and during treatment.
- Allergic reaction. If you’ve had an allergic reaction to imatinib oral tablets or any of their ingredients, you shouldn’t take these tablets. Ask your doctor what other medications are better options for you.
- Bleeding problems or blood cell disorders. If you have certain blood cell disorders, such as anemia, neutropenia, or thrombocytopenia, taking imatinib may worsen your condition. (With anemia you have a low level of red blood cells. With neutropenia, you have a low level of certain white blood cells. And with thrombocytopenia you have a low level of platelets.) Imatinib can cause hemorrhage (serious bleeding) and blood cell problems such as anemia, neutropenia, and thrombocytopenia. Tell your doctor if you have or have had bleeding problems or blood cell disorders. They’ll tell you if it’s safe for you to take imatinib. Your doctor will also monitor you for bleeding problems and blood cell disorders while you’re taking the drug.
- Kidney problems. Taking imatinib can worsen kidney function. If you have any kidney problems or conditions such as diabetes, congestive heart failure, or high blood pressure, tell your doctor. These conditions can increase your risk for kidney damage while you’re taking imatinib. Your doctor will check your kidney function before and during treatment with this drug.
- Gastrointestinal (GI) problems. If you have a stomach ulcer or another GI problem, taking imatinib may increase your risk for bleeding, and tears or holes in your stomach or intestines. Imatinib can also cause GI irritation and other serious GI problems. Tell your doctor if you have any GI problems. In some cases, it may not be safe for you to take imatinib.
- Hypothyroidism. If you have hypothyroidism and are taking medication for it, tell your doctor. (With hypothyroidism, your body doesn’t make enough thyroid hormones.) Your doctor will check your thyroid hormone levels before you start taking imatinib, and they’ll monitor the levels during treatment with the drug.
- Liver problems. If you have liver problems, taking imatinib may increase your risk for side effects of the drug. Ask your doctor about the safety of imatinib if you have liver disease or have had it in the past.
For more information about some of these conditions, see the “What are side effects of imatinib oral tablets?” section above.
Imatinib oral tablets and alcohol
There aren’t any known interactions between imatinib and alcohol. But drinking alcohol while taking imatinib may increase some side effects of the drug. These side effects may include:
- nausea
- diarrhea
- headache
- dizziness
- blurry vision
Drinking large amounts of alcohol can increase your risk for liver problems with imatinib treatment. This can make it take longer than usual for your body to clear imatinib.
If you drink alcohol, ask your doctor if it’s safe for you to drink during imatinib treatment. If your doctor confirms that you can, ask them how much is safe to drink.
Pregnancy and breastfeeding
It’s not safe to take imatinib if you’re pregnant. This drug may increase the risk of pregnancy loss and harm to an unborn fetus if it’s used during pregnancy.
If you’re a female* taking imatinib, you should use an effective form of birth control to help prevent pregnancy. And you should continue using birth control for at least 14 days after you stop treatment.
Ask your doctor if you’d like to know more about the risk of imatinib use during pregnancy and your need for birth control.
Imatinib does pass into breast milk. So you should avoid breastfeeding while you’re taking this drug and for at least 1 month after you stop treatment.
Your doctor can recommend ways other than breastfeeding to feed your child during imatinib treatment.
* In this article, we use the term “female” to refer to someone’s sex assigned at birth. For information about the difference between sex and gender, see this article.
Sprycel is a brand-name medication that contains the active drug dasatinib. This active drug isn’t available in a generic version. Imatinib is an active drug that comes as a generic medication and a brand-name drug called Gleevec.
Both dasatinib and imatinib are tyrosine kinase inhibitors. They work in similar ways to treat certain types of leukemia (blood cell cancers) in children and adults. They have some similar uses, side effects, and warnings.
See this detailed comparison for more information about how Gleevec and Sprycel compare. Also talk with your doctor about which drug is best for you.
Imatinib and nilotinib are both tyrosine kinase inhibitors.
They’re used to treat some similar types of leukemia (blood cell cancers) in adults and children. But they have some different uses as well. Imatinib and nilotinib have some similar side effects, risks, and drug interactions.
Tasigna is a brand-name version of the active drug nilotinib. This active drug isn’t available in a generic version. Imatinib is an active drug that comes as a generic medication and a brand-name drug called Gleevec.
If you’d like to learn more about how Gleevec compares with Tasigna, see this side-by-side overview. Talk with your doctor if you have more questions about these two medications and how they compare.
Don’t take more imatinib oral tablets than your doctor prescribes. Using more than this can lead to serious side effects.
Symptoms of overdose
Symptoms caused by an imatinib overdose can include:
- nausea and vomiting
- diarrhea
- rash
- edema (swelling, which may involve your face
- fatigue (lack of energy)
- fever
- muscle spasms
- pancytopenia (low level of red blood cells, platelets, and white blood cells)
- thrombocytopenia (low level of platelets)
- belly pain
- headache
- decreased appetite
What to do in case you take too much imatinib
Call your doctor if you think you’ve taken too many imatinib oral tablets. You can also call 800-222-1222 to reach the American Association of Poison Control Centers, or use its online resource. But if you have severe symptoms, immediately call 911 (or your local emergency number) or go to the nearest emergency room.
If you have a certain type of cancer, your doctor may prescribe imatinib oral tablets for you.
To learn more about the types of cancer imatinib is used to treat, see the “What are imatinib oral tablets used for?” section above.
You may have questions about your condition and how imatinib could work. Here are a few questions for you to consider asking your doctor:
- Do I need to follow a special diet while I’m taking imatinib?
- Will imatinib stop working for me after a while?
- Will I need to take other medications with imatinib?
- Is imatinib safe for me to take if I have chronic obstructive pulmonary disease (COPD)?
- Are there fruits and fruit juices other than grapefruit that I should avoid while I’m taking imatinib?
You can read this Healthline article to learn more about chronic myeloid leukemia treatment options other than imatinib.
Q:
Does imatinib have any long-term side effects?
Anonymous patientA:
Yes, it possibly does.
Both short- and long-term use of imatinib have caused liver damage and liver failure, leading to liver transplant and even death in some cases. Before you start taking imatinib and during treatment, your doctor will monitor your liver function.
Lasting reduced kidney function can also occur with imatinib. In studies, people taking imatinib for 1 year had reduced kidney function compared with when they started treatment. This may be reversible when imatinib is stopped.
You may have a higher risk for reduced kidney function if you already have kidney disease, diabetes, high blood pressure, or heart failure. Before starting imatinib and during treatment, your doctor will monitor your kidney function.
Before starting imatinib, be sure to let your doctor know about any medical conditions you have. Your doctor can monitor you as needed during treatment with this drug. And they can let you know if you’re at risk for any long-term side effects with imatinib.
Melissa Badowski, PharmD, MPH, FCCPAnswers represent the opinions of our medical experts. All content is strictly informational and should not be considered medical advice.Disclaimer: Healthline has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.