Cipro (ciprofloxacin) is a brand-name prescription antibiotic medication. It’s used to treat infections caused by bacteria.
Cipro belongs to a class of antibiotics called fluoroquinolones.
Cipro is effective for treating infections caused by many different types of bacteria. These include bacteria that cause infections in the urinary tract, abdomen, skin, prostate, and bone, as well as other types of infections.
Cipro comes in several forms:
- tablets (Cipro)
- extended-release tablets (Cipro XR)
- powder for oral suspension (Cipro)
Cipro can cause mild or serious side effects. The following list contains some of the key side effects that may occur while taking Cipro. This list does not include all possible side effects.
For more information on the possible side effects of Cipro, or tips on how to deal with a troubling side effect, talk with your doctor or pharmacist.
More common side effects
The more common side effects of Cipro include:
- nausea
- diarrhea
- vomiting
- upset stomach
- dizziness
- rash
Also, results from a liver function test can be higher than normal. This is usually temporary, but can also be a sign of liver damage.
Most of these side effects may go away within a few days or a couple of weeks. If they’re more severe or don’t go away, talk with your doctor or pharmacist.
Serious side effects
This is not common, but in some cases, Cipro can cause more serious side effects. Call your doctor right away if you have any serious side effects. Call 911 if your symptoms feel life threatening or if you think you’re having a medical emergency.
Serious side effects and their symptoms can include:
- Tearing or swelling in a tendon (tissue that connects muscle to bone). Symptoms can include:
- pain or swelling in the tendon by the heel of the foot, ankle, knee, hand or thumb, shoulder, or elbow
- Liver damage. Symptoms can include:
- stomach pain
- loss of appetite
- dark-colored urine
- yellowing of your skin or the whites of your eyes
- Severe allergic reaction. Symptoms can include:
- severe rash or hives
- trouble breathing or swallowing
- swelling of your lips, tongue, or face
- rapid heartbeat
- Mood changes. Symptoms can include:
- anxiety
- depression
- restlessness
- trouble sleeping
- hallucinations
- suicidal thoughts
- Seizures, tremors, or convulsions
- C. difficile infection (an intestinal infection that can be life threatening). Symptoms can include:
- severe diarrhea
- bloody stool
- stomach cramps
- fever
- Nerve problems in your arms, legs, feet, or hands. Symptoms can include:
- pain
- burning
- tingling
- numbness
- weakness
- Severe sunburn due to skin sensitivity to ultraviolet (UV) light
- Dangerously low blood sugar. This is more likely to happen in people ages 65 years and older and those with diabetes. Symptoms can include:
- dizziness
- confusion
- shakiness
- sweating
- weakness
- passing out
- coma
- Aortic aneurysm (bulging due to weakness in the aorta) or aortic dissection (a tear in the aorta), in people ages 65 years or older. Symptoms can include:
- sudden, severe pain in the stomach, chest, or back
- trouble speaking or walking
- shortness of breath
Due to these safety concerns, the
Other antibiotics should be used as a first choice.
Long-term side effects
Most Cipro side effects occur soon after the medication is taken. However, taking Cipro long-term may increase the risk of experiencing severe side effects. These long-term side effects can include tendon damage, liver damage, intestinal infection, and nerve problems.
Diarrhea
Diarrhea is a common side effect of antibiotics, including Cipro. About 2 to 5 percent of people who take Cipro have diarrhea.
Sometimes diarrhea can become severe with loose, watery stools, bloody stools, stomach cramps, and fever. In some cases, this may occur due to a C. difficile infection, which is caused by an imbalance of gut bacteria. This can be life threatening.
If you have severe diarrhea while taking Cipro, talk with your doctor right away. They may recommend treatment for it. In most cases, diarrhea typically goes away shortly after you stop taking Cipro.
Headache
Some people who take Cipro get headaches. In clinical studies, less than 1 percent of people had headaches while taking Cipro. These headaches are usually mild and may go away with continued use of the drug. If you get a headache that doesn’t go away while you’re taking Cipro, talk with your doctor.
Yeast infection
Vaginal yeast infections can sometimes occur after treatment with antibiotics, including Cipro. If you’ve never had a yeast infection before and think you might have one, see your doctor for a diagnosis and treatment.
Side effects in children
Cipro use is typically avoided in children because it might cause joint damage in children. Symptoms of joint damage in children can include reduced joint movement and joint pain. If your child is taking Cipro and has these symptoms, call their doctor right away.
Side effects in older adults
People ages 65 years and older are more likely than younger adults to have side effects from Cipro. However, the types of side effects they have are the same as those in younger adults, with one exception.
Adults ages 65 years or older have a risk of aortic aneurysm or aortic dissection with Cipro. Aortic aneurysm refers to bulging due to weakness in the aorta. This is the major blood vessel that transports blood out of your heart to the rest of your body. Aortic dissection is a tear in the aorta.
Symptoms of these conditions can include:
- sudden, severe pain in the stomach, chest, or back
- trouble speaking or walking
- shortness of breath
Be sure to talk with your doctor about your risk of side effects with Cipro.
Suicide prevention
If you know someone at immediate risk of self-harm, suicide, or hurting another person:
- Ask the tough question: “Are you considering suicide?”
- Listen to the person without judgment.
- Call 911 or the local emergency number, or text TALK to 741741 to communicate with a trained crisis counselor.
- Stay with the person until professional help arrives.
- Try to remove any weapons, medications, or other potentially harmful objects.
If you or someone you know is having thoughts of suicide, a prevention hotline can help. The 988 Suicide and Crisis Lifeline is available 24 hours a day at 988. During a crisis, people who are hard of hearing can use their preferred relay service or dial 711 then 988.
Cipro is available as a generic drug. The generic drug name is ciprofloxacin.
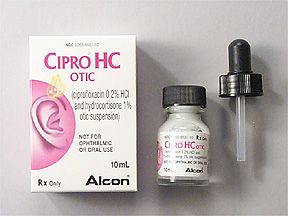
Ciprofloxacin (generic Cipro) is available in several forms, including:
- oral immediate-release tablet*
- oral extended-release tablet*
- ophthalmic solution (eye drops)
- otic solution (ear drops)
- oral suspension
- solution for injection
* Immediate release means the drug is released into your body right away after taking a dose. Extended release means the drug is released gradually over time.
The Food and Drug Administration (FDA) approves medications, such as Cipro, to treat certain conditions.
Approved uses for Cipro
Cipro is FDA-approved for treating many different types of infections in adults. Examples of these FDA-approved uses include:
- Abdominal infections such as:
- gastroenteritis (including diarrhea caused by infection)
- respiratory infections such as:
- Sexually transmitted diseases (STDs) such as gonorrhea
- Sinus infection
- Skin infections such as cellulitis
- Urinary tract infections (UTIs) such as:
Less common FDA-approved uses include:
Cipro XR extended-release tablets are only approved for treating UTIs.
Although Cipro is effective, the
- sinus infections
- bronchitis
- UTIs
For these conditions, the risk of serious side effects caused by Cipro outweigh the benefits. Other antibiotics should be used as a first choice.
Uses that are not approved
Cipro is also sometimes used off-label for uses that are not approved by the FDA. Examples of these include:
- blood infection
- chlamydia
- cystic fibrosis
- sore throat or strep throat (Cipro is rarely used for these conditions)
- tooth infection
- traveler’s diarrhea
Uses for ciprofloxacin
The generic version of Cipro is approved to treat all of the conditions that Cipro is approved for. In addition to those conditions, ciprofloxacin is approved to treat ear infections.
Cipro for children
Cipro is FDA-approved for use in children to treat certain infections, such as severe UTIs. However, Cipro is not the first choice for use in children due to concerns that it may cause joint damage in children.
The American Academy of Pediatrics recommends that Cipro and other fluoroquinolone antibiotics only be used to treat children when there’s no other safe or effective option.
The Cipro dosage your doctor prescribes will depend on several factors. These include:
- the type and severity of the condition you’re using Cipro to treat
- your age
- the form of Cipro you take
- other medical conditions you may have, such as kidney disease
Typically, your doctor will start you on a low dosage and adjust it over time to reach the dosage that’s right for you. They’ll ultimately prescribe the smallest dosage that provides the desired effect.
The following information describes dosages that are commonly used or recommended. However, be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosage to suit your needs.
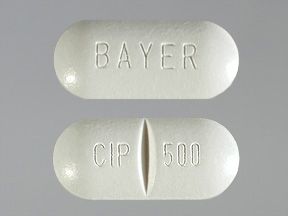
Drug forms and strengths
- tablets (Cipro): 250 mg, 500 mg, 750 mg
- extended-release* tablets (Cipro XR): 500 mg, 1,000 mg
- powder for oral suspension (Cipro): 250 mg/5 mL, 500 mg/5 mL
* Extended release means the drug is released gradually over time.
General dosage information
The typical dosage for immediate-release Cipro is 250 to 750 mg every 12 hours for up to 14 days. Your doctor will determine the best form and dosage of Cipro for your condition.
Dosage for UTI
The typical dosage for urinary tract infections (UTIs) is 250 to 500 mg every 12 hours for 3 to 14 days.
Dosage for bone and joint infections
The typical dosage for bone and joint infections is 500 to 750 mg every 12 hours for 4 to 8 weeks.
Dosage for diarrhea caused by infection
The typical dosage for diarrhea caused by infection is 500 mg every 12 hours for 5 to 7 days.
Dosage for respiratory infections
The typical dosage for respiratory infections is 500 to 750 mg every 12 hours for 7 to 14 days.
Dosage for sinus infections
The typical dosage for sinus infections is 500 mg every 12 hours for 10 days.
Dosage for abdominal infections
The typical dosage for abdominal infections is 500 mg every 12 hours for 7 to 14 days.
Children’s dosage
For children ages 1–17 years of age, the typical dosage is 10 to 20 mg/kg every 12 hours for 7 to 21 days. The dosage should not be greater than 750 mg every 12 hours.
Dosage for Cipro XR
Cipro XR extended-release tablets are only approved for treating urinary tract infections (UTIs).
- Typical dosage: 500 mg once daily for 3 days.
- Typical dosage for severe UTIs: 1,000 mg once daily for 7 to 14 days.
Special dosage considerations
If you have kidney disease, your doctor may prescribe Cipro at a lower dose or have you take the medication less frequently.
What if I miss a dose?
If you miss a dose, take it as soon as you can. However, if there are 6 hours or less before your next dose, skip the missed dose and take your next dose as scheduled.
Never try to catch up by taking two doses at a time. This can cause dangerous side effects.
Cipro can interact with several other medications. It can also interact with certain supplements as well as certain foods.
Different interactions can cause different effects. For instance, some can interfere with how well a drug works, while others can cause increased side effects.
In addition to the information below, you can also see this detailed article about Cipro’s interactions.
Cipro and other medications
Below is a list of medications that can interact with Cipro. This list does not contain all drugs that may interact with Cipro.
Before taking Cipro, be sure to tell your doctor and pharmacist about all prescription, over-the-counter, and other drugs you take. Also tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you avoid potential interactions.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
Antacids
Many antacids (such as Tums, Gaviscon, and Maalox) contain calcium carbonate, magnesium hydroxide, and aluminum hydroxide. These ingredients can bind to Cipro and prevent your body from absorbing it. This can decrease how well Cipro works.
To avoid this interaction, take Cipro at least two hours before taking an antacid, or six hours afterward.
Anticoagulant drugs
Taking Cipro with oral anticoagulant drugs such as warfarin (Coumadin, Jantoven) might increase the anticoagulant effects. This might result in increased bleeding. If you take an anticoagulant, your doctor may need to monitor your bleeding risk more frequently if you take Cipro.
Drugs that prolong the QT interval
Certain medications prolong your QT interval, which means they might affect the rhythm of your heartbeat. Taking Cipro with these drugs can increase the risk of having a dangerous irregular heartbeat. Cipro should be avoided or used very carefully with these medications.
Examples of these medications include:
- amiodarone (Pacerone)
- antipsychotic medications such as haloperidol, quetiapine (Seroquel, Seroquel XR), and ziprasidone (Geodon)
- macrolide antibiotics such as erythromycin (Ery-Tab) and azithromycin (Zithromax)
- quinidine
- procainamide
- tricyclic antidepressants such as amitriptyline, desipramine (Norpramin), and imipramine (Tofranil)
- sotalol (Sotylize, Betapace, Betapace AF, Sorine)
Clozapine
Taking Cipro with clozapine (Versacloz, Fazaclo ODT) can increase the levels of clozapine in the body and increase the risk of clozapine side effects.
Diabetes drugs
Cipro can increase the blood sugar-lowering effects of certain diabetes drugs, such as glyburide (Diabeta, Glynase PresTabs) and glimepiride (Amaryl). This might cause blood sugar levels to become too low.
Methotrexate
Taking Cipro with methotrexate (Rasuvo, Otrexup) can increase the levels of methotrexate in your body and increase the risk of methotrexate side effects.
Probenecid
Probenecid can increase Cipro levels in the body and increase the risk of Cipro side effects.
Ropinirole
Taking Cipro with ropinirole (Requip, Requip XL) can increase the levels of ropinirole in the body and increase the risk of ropinirole side effects.
Phenytoin
Taking Cipro with the seizure drug phenytoin (Dilantin, Dilantin-125, Phenytek) can cause phenytoin levels in the body to become too low. This can result in uncontrolled seizures in people taking phenytoin for epilepsy.
Sildenafil
Taking Cipro with sildenafil (Viagra, Revatio) can increase the levels of sildenafil in your body and increase the risk of sildenafil side effects.
Theophylline
Taking Cipro with theophylline can increase levels of theophylline in your body. This can cause serious theophylline side effects. These include nausea, vomiting, jitters, irritability, abnormal heartbeat, heart attack, seizures, and breathing failure. Cipro and theophylline should not be taken together if possible.
Tizanidine
Cipro can increase the sedative and blood pressure effects of tizanidine (Zanaflex). Cipro and tizanidine should not be taken together.
Zolpidem
Cipro can increase the levels of zolpidem (Ambien, Ambien CR, Edluar, Intermezzo) in the body. This might result in excessive sedation from zolpidem.
Metronidazole
Cipro can prolong your QT interval, which means it might affect the rhythm of your heartbeat. In rare cases, metronidazole (Flagyl, Flagyl ER) might also cause QT interval prolongation. Using these drugs together might increase the risk of a dangerous irregular heartbeat.
Talk with your doctor before using these drugs together.
Tylenol
There are no known interactions between Cipro and Tylenol (acetaminophen).
Tinidazole
There are no known interactions between Cipro and tinidazole.
Cipro and herbs and supplements
Some vitamin and supplement products can bind to Cipro and prevent your body from absorbing it. This can decrease how well Cipro works. These supplements include:
- multivitamins
- calcium
- iron
- zinc
To avoid this interaction, you should take Cipro at least two hours before you take these supplements, or at least six hours afterward.
Cipro and foods
Cipro can interact with certain foods.
Cipro and dairy or milk
Dairy foods or calcium-fortified juice can bind to Cipro and prevent your body from absorbing it. This can decrease how well Cipro works. To avoid this interaction, you should take Cipro at least two hours before you consume these foods, or at least two hours afterward.
Cipro and caffeine
Cipro can increase the effects of caffeine consumed from coffee, tea, chocolate, and other sources. This might increase the risk of caffeine-related side effects such as nervousness, jitteriness, and trouble sleeping.
Cipro and alcohol
Taking Cipro with alcohol will not make the antibiotic less effective, but the combination might increase the risk of certain side effects or make side effects worse. Examples of side effects that might be more likely to occur, or worsened by alcohol use, include:
- nausea
- vomiting
- dizziness
- upset stomach
- liver problems
Here are answers to some common questions about Cipro.
Will I need to use Cipro long term?
In most cases, Cipro treatment is short term, from 3 to 14 days. But for some infections, such as certain bone or joint infections, treatment may last several weeks.
Does Cipro make you tired?
Cipro does not usually cause you to feel tired, but in some cases, people report feeling tired while taking it. It’s common for people who have infections to feel fatigued or more tired than usual. Feeling more tired than usual may be due to your condition rather than the medication.
Is Cipro safe to take?
Cipro has been shown to be a safe and effective treatment for bacterial infections.
Before you start Cipro treatment, you and your doctor will discuss your medical history. This includes all of the medical conditions you have and the drugs you’re taking. Reviewing these and other factors will help you and your doctor determine if Cipro is safe for you to take.
You and your doctor will also discuss all possible side effects of Cipro before you start treatment.
If you’re taking Cipro and you’re concerned about the drug’s safety, be sure to talk with your doctor.
Is Cipro an antibiotic?
Yes, Cipro is an antibiotic.
Is Cipro a type of penicillin?
No, Cipro is not a penicillin. Cipro is a fluoroquinolone antibiotic.
You may wonder how other antibiotics compare to Cipro.
Cipro vs. Bactrim
Cipro and Bactrim are both antibiotic drugs, but they belong to different drug classes. Cipro is a fluoroquinolone antibiotic. Bactrim is a sulfonamide antibiotic. Bactrim contains two drugs in one pill, trimethoprim and sulfamethoxazole.
Use
Cipro and Bactrim can be used for treating urinary tract infections (UTIs).
Dosage and forms
Cipro is available as an oral tablet and oral suspension that are taken twice daily. Cipro XR extended-release tablets are taken once daily. Bactrim is available as oral tablets and an oral suspension that are also taken twice daily.
Effectiveness
Both Cipro and Bactrim are effective for treating UTIs. However, Cipro is not a first-choice medication for this condition, due to the risk of serious side effects. Cipro should only be used for UTIs when first-choice medications cannot be used.
According to the Infectious Diseases Society of America, Bactrim is usually a first-choice antibiotic for treating UTIs.
When comparing drugs, keep in mind that your doctor will make treatment recommendations based on your individual needs. They’ll consider several factors, such as the location of your infection, bacteria that might be causing your infection, and bacterial resistance rates in your geographic area.
They’ll also consider your age, gender, whether you’re planning to become pregnant, other conditions you may have, your risk of side effects, and how severe your condition is.
Side effects and risks
Cipro and Bactrim cause similar common side effects such as:
- nausea
- diarrhea
- vomiting
- upset stomach
- dizziness
- rash
People with a sulfa allergy should not take Bactrim.
Cipro is not a first-choice antibiotic for urinary tract infections due to the potential for serious side effects. These include tendon, joint, and nerve damage, and central nervous system side effects.
Costs
Cipro and Bactrim are both brand-name drugs. They’re both also available in generic forms. Generic drugs usually cost less than brand-name drugs. The generic name of Bactrim is trimethoprim-sulfamethoxazole.
Brand-name Cipro is usually more expensive than brand-name Bactrim. The generic forms of these medications cost about the same. The actual amount you pay will depend on your insurance.
Cipro vs. Macrobid
Cipro and Macrobid (nitrofurantoin) are both antibiotic drugs, but they belong to different drug classes. Cipro is a fluoroquinolone antibiotic. Macrobid is a nitrofuran antibiotic.
Use
Cipro and Macrobid can be used to treat urinary tract infections (UTIs). However, Macrobid is only for mild or uncomplicated UTIs. It should not be used for more severe UTIs or kidney infections.
Cipro is sometimes used for more severe UTIs or kidney infections, but it’s not a first-choice antibiotic due to the risk of serious side effects.
Dosage and forms
Cipro is available as an oral tablet and oral suspension that are taken twice daily. Cipro XR extended-release tablets are taken once daily. Macrobid is available as an oral capsule that’s taken twice daily.
Effectiveness
Both Cipro and Macrobid are effective for treating mild or uncomplicated urinary tract infections. However, according to the Infectious Diseases Society of America, Macrobid is usually a first-choice antibiotic for treating urinary tract infections.
Cipro should only be used for urinary tract infections when first-choice medications cannot be used. Cipro is not a first-choice medication for urinary tract infections due to the risk of serious side effects.
When comparing drugs, keep in mind that your doctor will make treatment recommendations based on your individual needs. They’ll consider several factors, such as the location of your infection, bacteria that might be causing your infection, and bacterial resistance rates in your area.
They’ll also consider your age, gender, whether you’re planning to become pregnant, other conditions you may have, your risk of side effects, and how severe your condition is.
Side effects and risks
Cipro and Macrobid have some similar side effects, and some that differ. Below are examples of these side effects.
| Both Cipro and Macrobid | Cipro | Macrobid | |
| More common side effects | • nausea • headache • flatulence • rash • upset stomach • dizziness | (no unique common side effects) | (no unique common side effects) |
| Serious side effects | • nerve damage | • tendon damage • joint damage • central nervous system side effects | • liver damage • lung damage |
Costs
Cipro and Macrobid are both brand-name drugs. They’re both also available in generic forms. Generic drugs usually cost less than brand-name drugs. The generic name of Macrobid is nitrofurantoin.
Brand-name Cipro is usually more expensive than brand-name Macrobid. The generic form of Macrobid is usually more expensive than generic Cipro. The actual amount you pay will depend on your insurance.
Cipro vs. levofloxacin (Levaquin)
Cipro and levofloxacin are both fluoroquinolone antibiotics.
Levofloxacin is an active drug that’s available as a generic medication. It used to be available as the brand-name medication Levaquin, which has been discontinued.
Use
Cipro and levofloxacin are FDA-approved for many similar uses. Examples of these include:
- urinary tract infection
- pneumonia
- skin infections
- sinus infection
- prostate infection
Cipro is also FDA-approved to treat abdominal and bone and joint infections.
Dosage and forms
Cipro is available as an oral tablet and oral suspension that are taken twice daily. Cipro XR extended-release tablets are taken once daily.
Levofloxacin is available as an oral tablet that’s taken once daily.
Effectiveness
Both Cipro and levofloxacin are effective for their FDA-approved uses. However, the
- sinus infections
- bronchitis
- urinary tract infections
For these conditions, the risk of serious side effects caused by Cipro and levofloxacin outweigh their benefits. Other antibiotics should be used as a first choice.
When comparing drugs, keep in mind that your doctor will make treatment recommendations based on your individual needs. They’ll consider several factors, such as the location of your infection, bacteria that might be causing your infection, and bacterial resistance rates in your area.
They’ll also consider your age, gender, childbearing potential, other conditions you may have, your risk of side effects, and how severe your condition is.
Side effects and risks
Cipro and levofloxacin have similar common and serious side effects.
The more common side effects of Cipro and levofloxacin include:
- nausea
- diarrhea
- vomiting
- upset stomach
- dizziness
- rash
Cipro and levofloxacin can also cause similar serious side effects including:
- tendon tearing or swelling
- liver damage
- severe allergic reaction
- mood changes
- seizures, tremors, or convulsions
- intestinal infection
- nerve problems
- aortic aneurysm or aortic dissection, in people ages 65 and older
Because of these serious side effects, Cipro and levofloxacin are not often considered first-choice antibiotics.
Costs
Cipro is a brand-name drug that’s also available in generic form. Levofloxacin is a generic drug. Generic drugs usually cost less than brand-name drugs. The generic form of Cipro and levofloxacin cost about the same. The actual amount you pay will depend on your insurance.
Cipro vs. cephalexin (Keflex)
Cipro and cephalexin are both antibiotics, but they belong to different drug classes. Cipro is a fluoroquinolone antibiotic. Cephalexin is a cephalosporin antibiotic.
Cephalexin is an active drug that’s available as a generic medication. It used to be available as the brand-name medication Keflex, which has been discontinued.
Use
Cipro and cephalexin are both FDA-approved to treat some similar infections. Examples of these include:
- urinary tract infection
- pneumonia
- skin infections
- prostate infection
- bone and joint infections
Cipro is also FDA-approved for abdominal infections.
Drug forms
Cipro is available as an oral tablet and oral suspension that are taken twice daily. Cipro XR extended-release tablets are taken once daily.
Cephalexin is available as an oral capsule that’s taken two to four times daily.
Effectiveness
Cipro and cephalexin are both effective for their FDA-approved uses. However, they’re not always considered a first-choice antibiotic. This may be because they’re less studied than other medications, or it may be due to the risk of side effects.
The
- sinus infections
- bronchitis
- urinary tract infections
For these conditions, the risk of serious side effects caused by Cipro outweigh its benefits. Other antibiotics should be used as a first choice.
When comparing drugs, keep in mind that your doctor will make treatment recommendations based on your individual needs. They’ll consider several factors, such as the location of your infection, bacteria that might be causing your infection, and bacterial resistance rates in your area.
They’ll also consider your age, gender, whether you’re planning to become pregnant, other conditions you may have, your risk of side effects, and how severe your condition is.
Side effects and risks
Cipro and cephalexin have some similar common and serious side effects. Examples of these side effects are included below.
| Both Cipro and cephalexin | Cipro | cephalexin | |
| More common side effects | • nausea • diarrhea • vomiting • upset stomach or stomach pain • dizziness • rash • headache | (no unique common side effects) | (no unique common side effects) |
| Serious side effects | • liver damage • severe allergic reaction • seizures, tremors, or convulsions • intestinal infections | • tendon damage • mood changes • nerve problems | (no unique serious side effects) |
Costs
Cipro is a brand-name drug that’s also available in generic form. Cephalexin is a generic drug. Generic drugs usually cost less than brand-name drugs. The generic form of Cipro and cephalexin cost about the same. The actual amount you pay will depend on your insurance.
As with all medications, the cost of Cipro can vary. The actual price you’ll pay depends on your insurance plan coverage, your location, and the pharmacy you use.
Keep in mind that you may be able to get a 90-day supply of Cipro. If approved by your insurance company, getting a 90-day supply of the drug could reduce your number of trips to the pharmacy and help lower the cost. If you’re interested in this option, check with your doctor, pharmacist, or insurance company.
Before approving coverage for Cipro, your insurance company may require you to get prior authorization. This means that your doctor and insurance company will need to communicate about your prescription before the insurance company will cover the drug. The insurance company will review the prior authorization request and decide if the drug will be covered.
If you’re not sure if you’ll need to get prior authorization for Cipro, contact your insurance company.
Financial and insurance assistance
If you need financial support to pay for Cipro, or if you need help understanding your insurance coverage, help is available.
Financial assistance in helping you pay for Cipro may be available. You can search Medicine Assistance Tool and NeedyMeds to find programs that may help decrease Cipro’s cost. To learn more, visit their websites.
To learn more about saving money on prescriptions, check out this article.
Mail-order pharmacies
Cipro may be available through a mail-order pharmacy. Using this service may help lower the drug’s cost and allow you to get your medication without leaving home.
If recommended by your doctor, you may be able to receive a 90-day supply of Cipro, so there’s less concern about running out of the medication. If you’re interested in this option, check with your doctor, pharmacist, or insurance company. Some Medicare plans may help cover the cost of mail-order medications.
If you don’t have insurance, you can ask your doctor or pharmacist about online pharmacy options.
Generic version
Cipro is available as the generic drug ciprofloxacin. Ciprofloxacin is available in several forms (see “Cipro generic name” above for details).
A generic drug is an exact copy of the active drug in a brand-name medication. The generic is considered to be as safe and effective as the original drug. And generics tend to cost less than brand-name drugs.
If your doctor has prescribed Cipro and you’re interested in using ciprofloxacin instead, talk with your doctor. They may have a preference for one version or the other. You’ll also need to check your insurance plan, as it may only cover one or the other.
Take Cipro exactly according to your doctor’s instructions. You might start to feel better before you finish your entire Cipro treatment. Even if you start to feel better, do not stop taking Cipro. In many cases, it’s important to finish the entire treatment to make sure the infection doesn’t come back.
If you’re feeling better and want to stop Cipro early, be sure to talk with your doctor first to make sure it’s safe to do so.
Timing
Cipro tablets and suspension should be taken at about the same time each day in the morning and the evening.
Cipro XR extended-release tablets should be taken once daily at about the same time each day.
Taking Cipro with food
Cipro can be taken with or without food. Either way you take it, be sure to drink plenty of fluids while taking Cipro.
Cipro should not be taken along with dairy products or calcium-fortified juices. It should be taken at least two hours before or after consuming these products. However, Cipro can be taken along with a meal that contains dairy products or calcium-fortified foods or drinks.
Can Cipro be crushed, chewed, or split?
No, you should not crush or chew Cipro or Cipro XR extended-release tablets.
Cipro tablets can be split in half, if needed. However, Cipro XR extended-release tablets should not be split. Cipro XR should be swallowed whole.
Cipro suspension should be shaken well before you take it.
If you have concerns about swallowing your medication, talk with your doctor about ways to make Cipro easier to swallow. This article also has some tips on swallowing pills.
Cipro is FDA-approved for use in children to treat certain infections, such as severe urinary tract infections (UTIs). The typical dosage for children ages 1–17 years is 10–20 mg/kg every 12 hours for 7 to 21 days. The dosage should not be more than 750 mg every 12 hours.
Even though Cipro is FDA-approved for use in children, it’s not the first choice. In fact, it’s usually avoided in children due to concerns that it may damage joints in children.
The American Academy of Pediatrics recommends that Cipro and other fluoroquinolone antibiotics only be used to treat children when there’s no other safe or effective alternative.
There haven’t been enough studies done in pregnant humans to be sure how this drug might affect a fetus. Some
Talk with your doctor if you’re pregnant or planning to become pregnant. This medication should be used during pregnancy only if the benefit justifies the potential risk.
You should not breastfeed while taking this medication. Cipro can pass through breast milk and cause side effects in a child who is breastfed.
Tell your doctor if you’re breastfeeding. You may need to decide whether to stop breastfeeding or stop taking this medication.
Taking too much Cipro can increase your risk of harmful or serious side effects.
Overdose symptoms
Symptoms of an overdose of Cipro can include:
- nausea
- diarrhea
- vomiting
- upset stomach
- dizziness
- anxiety
- liver damage
- kidney damage
- nerve damage
- tendon damage
What to do in case of overdose
If you think you’ve taken too much of this drug, call your doctor or seek guidance from the American Association of Poison Control Centers at 800-222-1222 or through its online tool. But if your symptoms are severe, call 911 or go to the nearest emergency room right away.
Cipro is an antibiotic in the class of fluoroquinolones. This type of antibiotic is bactericidal. This means that it directly kills bacteria. It does this by blocking enzymes that are needed for bacteria survival.
Cipro is a broad-spectrum antibiotic. This means it works against many different types of bacteria. However, many bacteria have grown to be resistant to Cipro. Resistant bacteria can no longer be treated with a certain drug.
How long does it take to work?
Cipro begins to work against bacterial infections within hours of when you take it. However, you may not notice improvement in your symptoms for a few days.
There are many different antibiotics that are used as alternatives to Cipro. The most appropriate antibiotic to use can depend on your age, site of the infection, the type of bacteria causing the infection, drug allergies you may have, and the geographic region you live in.
If you’re interested in alternatives to Cipro, talk with your doctor about other antibiotic options that might be appropriate for you.
Note: Some of the drugs listed here are used off-label to treat these specific infections.
Alternatives for abdominal infections
Examples of other drugs that may be used to treat abdominal infections include:
- levofloxacin
- moxifloxacin (Avelox)
- metronidazole (Flagyl, Flagyl ER)
Alternatives for bone and joint infections
Examples of other drugs that may be used to treat bone and joint infections include:
- aztreonam (Azactam)
- ceftriaxone
- ertapenem (Invanz)
- levofloxacin
- metronidazole (Flagyl, Flagyl ER)
- piperacillin-tazobactam
- vancomycin
Alternatives for diarrhea caused by infection
Examples of other drugs that may be used to treat diarrhea caused by infection include:
- metronidazole (Flagyl, Flagyl ER)
- vancomycin
Alternatives for respiratory infections
Examples of other drugs that may be used to treat respiratory infections include:
- amoxicillin
- amoxicillin-clavulanate
- azithromycin (Zithromax)
- doxycycline (Acticlate, Doryx, Doryx MPC)
- levofloxacin
- moxifloxacin (Avelox)
- penicillin VK
Alternatives for sinus infection
Examples of other drugs that may be used to treat sinus infection include:
- amoxicillin
- amoxicillin-clavulanate
- doxycycline (Acticlate, Doryx, Doryx MPC)
- levofloxacin
Alternatives for skin infections
Examples of other drugs that may be used to treat skin infections include:
- amoxicillin
- cephalexin
- clindamycin
- doxycycline (Acticlate, Doryx, Doryx MPC)
- trimethoprim-sulfamethoxazole (Bactrim)
Alternatives for urinary tract infection
Examples of other drugs that may be used to treat urinary tract infections (UTIs) include:
- cefpodoxime
- cephalexin
- levofloxacin
- nitrofurantoin (Macrobid, Macrodantin)
- trimethoprim-sulfamethoxazole (Bactrim)
Cipro is sometimes prescribed by veterinarians to treat infections in dogs and cats. It’s commonly used for urinary tract infections (UTIs) and may also be used for other kinds of infections.
If you think your dog or cat has an infection, see your veterinarian for an evaluation and treatment. Different doses are used for animals than humans, so do not try to treat your pet with a Cipro prescription intended for humans.
If you think your pet has eaten your prescription of Cipro, call your veterinarian right away.
Cipro and other fluoroquinolone antibiotics can cause a falsely positive result for opioids on urine drug screenings. If you’re taking Cipro, consider disclosing this information before completing a drug screening.
How long Cipro stays in your system varies from person to person, but it’s usually one to two days.
Before taking Cipro, talk with your doctor about your health history. Cipro may not be appropriate for you if you have certain medical conditions.
For people with diabetes: Cipro and other fluoroquinolones can sometimes cause severe low blood sugar. This is more likely to happen in those with diabetes who are taking hypoglycemic drugs. You may need to monitor your blood sugar levels more closely if you take Cipro.
If your blood sugar gets too low, call your doctor. You may need to stop taking Cipro.
For people with myasthenia gravis: Cipro and other fluoroquinolone antibiotics can worsen muscle weakness in people with this condition. If you have myasthenia gravis, you should not take Cipro.
For people with QT interval prolongation: People with QT interval prolongation have a higher risk of having a potentially serious irregular heartbeat. Taking Cipro might worsen this condition, resulting in a life threatening arrhythmia.
Sun exposure: Cipro can make your skin more sensitive to sunlight. You may be more likely to get a severe sunburn while taking Cipro.
For people with an aortic aneurysm or risk factors for this condition: If you have an aortic aneurysm or if you’re ages 65 years or older, talk with your doctor about this before starting Cipro. An aortic aneurysm is bulging due to weakness in your aorta (the major blood vessel that transports blood out of your heart to the rest of your body). Having this condition, or risk factors for it, can increase your risk of aortic dissection (a tear in your aorta) during or after Cipro treatment. If you’re ages 65 years or older, you may be at increased risk of aortic aneurysm or dissection. Your doctor may recommend a treatment other than Cipro.
When Cipro is dispensed from the pharmacy, the pharmacist will add an expiration date to the label on the bottle. This date is typically one year from the date the medication was dispensed. Oral suspensions often have a much earlier expiration date.
The purpose of such expiration dates is to guarantee the effectiveness of the medication during this time. The Food and Drug Administration (FDA) advises to avoid using expired medications.
How long a medication remains good can depend on many factors, including how and where the medication is stored. Cipro should be stored at room temperature in its original container.
If you have unused medication that has gone past the expiration date, talk with your pharmacist about whether you might still be able to use it.
The following information is provided for clinicians and other healthcare professionals.
Mechanism of action
Cipro is a fluoroquinolone antibiotic that has bactericidal effects through inhibition of bacteria DNA gyrase and topoisomerase IV. These enzymes are required for bacterial DNA replication, transcription, repair, and recombination.
Pharmacokinetics and metabolism
The bioavailability of Cipro is about 70 percent when taken orally. Maximum blood concentrations occur within one to two hours.
Food delays Cipro tablet absorption, resulting in peak levels occurring closer to two hours, but does not delay absorption of Cipro suspension. However, food does not change overall absorption and peak levels of Cipro tablet or suspension.
About 40 percent to 50 percent of Cipro is excreted in the urine unchanged. Urinary excretion of Cipro is complete within about 24 hours after dosing.
The half-life of Cipro is about four to five hours for adults and children. In people with reduced kidney function, it may increase to six to nine hours.
Contraindications
Cipro is contraindicated in people with a history of hypersensitivity to Cipro or to any other fluoroquinolone antibiotic.
Concomitant administration with tizanidine is also contraindicated due to potentiation of sedative and hypotensive effects of tizanidine.
Storage
Cipro tablets should be stored at room temperature between 68°F and 77°F (20°C and 25°C).
Reconstituted Cipro suspension should also be stored at room temperature for up to 14 days. The suspension should not be frozen.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.