There are four types of mastectomies: total, skin-sparing, nipple-sparing, and modified radical. Many factors influence whether one type may be more beneficial for you than another. A healthcare professional can discuss your options.
A mastectomy is a surgery to remove the breast. Although a mastectomy is usually performed to treat breast cancer, it may also be performed as a preventive measure in people who have a high risk of the disease.
Many people can go home on the same day of the procedure, while others may spend a night or two in the hospital immediately following the surgery. It ultimately depends on whether reconstruction is performed and if there are any complications.
Recovery from a mastectomy can take several weeks. Most people can expect about 4 weeks to recover. During this time, your movement and activities are limited.
Your recovery period may be longer if you have any reconstruction immediately following the mastectomy.
Talk with your surgeon about what you can expect from recovery. Doing so allows you to set realistic expectations about returning to your everyday activities.
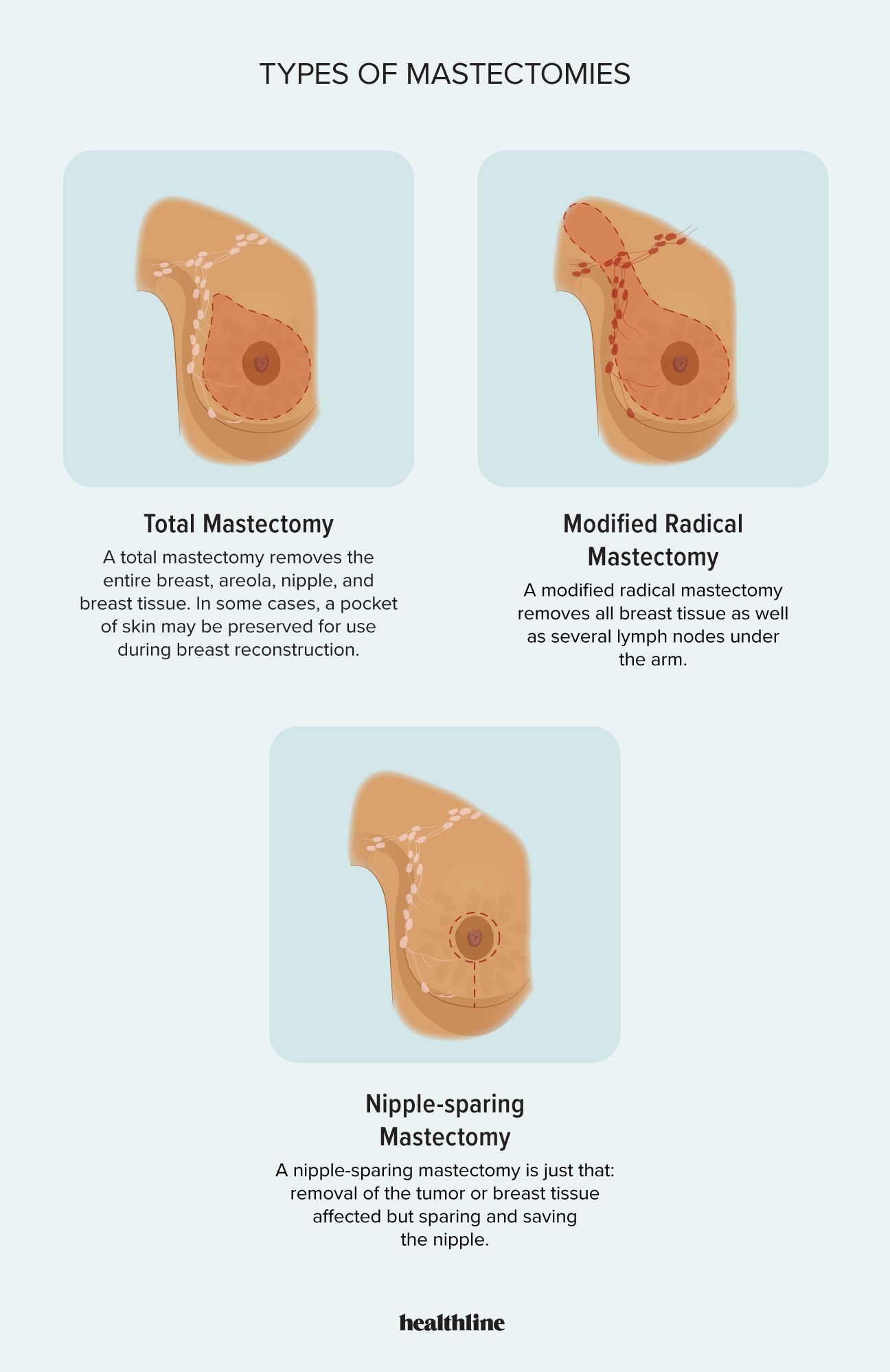
A total mastectomy is also known as a simple mastectomy. Its focus is to remove all the breast tissue, including the nipple and areola.
A total mastectomy may also be referred to as a “skin-sparing” mastectomy if reconstruction is also performed. This is because a skin pocket is preserved for use during reconstruction.
Your surgeon will not typically remove nearby lymph nodes unless the lymph nodes are within the breast tissue they need to remove. Likewise, no chest muscles or tissue beneath the breast are removed during this type of mastectomy.
Some people get this surgery as a preventive measure. In these cases, a surgeon removes the whole breast to reduce the risk of breast cancer in people who are considered high risk. You may choose to do this to both breasts, which is known as a double mastectomy.
During a modified radical mastectomy, your surgeon removes all breast tissue and several lymph nodes under the arm. The lymph nodes will likely be tested to see whether breast cancer has spread beyond the breast tissue.
In a modified radical mastectomy, no muscles below the breast are removed. As with a total mastectomy, those muscles remain intact.
This type of mastectomy is often an option for people who have invasive breast cancer or for people whose doctors expect to find a higher stage cancer.
About breast cancer staging
Doctors divide breast cancer into stages based on the size of the tumor and how much it has spread. Breast cancers that are large or have spread to nearby tissues or organs are at a higher stage than cancers that are small or still contained within the breast.
As the name suggests, a nipple-sparing mastectomy aims to remove all the breast tissue while leaving the nipple intact. However, if any of the tissue surrounding the nipple or areola shows signs of cancer, your surgeon may need to remove these, too.
This type of mastectomy is typically only an option for people who have early stage breast cancer with a smaller tumor.
Despite preserving the nipple during surgery, you may lose feeling and sensitivity. It’s worth speaking with your doctor about the pros and cons of preserving the nipple during a mastectomy.
Some people refer to a lumpectomy as a partial mastectomy, but that’s a misnomer.
A lumpectomy is a surgery that removes the cancerous part of the breast tissue and some of the healthy tissue around the tumor. However, it does not remove all the breast tissue.
Mastectomy is surgery to remove the entire breast.
You might get a lumpectomy if you have early stage cancer that has not spread beyond the original cancerous site.
After cancerous breast tissue is removed, you may be thinking about restoring your breast’s shape. People who have had a mastectomy often want to restore the breast mound, but it’s also not uncommon to skip the restoration and “go flat” instead.
If you decide to go with reconstruction, know that you don’t have to do so immediately. You can put off reconstruction for days, months, or even years.
If you’re undergoing any other breast cancer treatments, like radiation or chemotherapy, you may decide to postpone reconstruction until those treatments are done.
Reconstruction has several forms. Some people may opt for a full silicone implant for their breast reconstruction.
In other cases, a plastic surgeon may be able to use body fat, muscle, and tissue from another part of your body to rebuild a breast. Nipple reconstruction is also possible for some people.
If you don’t get reconstruction, you can also choose to use a breast prosthesis. Several options are available, each with its own pros and cons.
A prosthesis may be an ideal first step for some people unsure if they’d like a more long-term solution like reconstructive surgery.
You can also use a prosthesis if you’re undergoing other breast cancer treatments and are not ready for reconstructive surgery yet.
Types of breast prostheses include:
- External silicone breast prosthesis: These forms are designed to match your natural breast tissue’s weight. This can make you feel more balanced and even improve posture or balance after a mastectomy.
- Nonsilicone breast prosthesis: These lightweight forms are often made from foam or fiberfill material. These prostheses are ideal for use with exercise, swimming, and on hot days.
- Soft form in camisole: This prosthesis is a removable breast worn inside a camisole, a stretchy top often worn under blouses. You can also pull a camisole over your hips if you have trouble lifting clothes over your arms.
- Attachable breast: You can use a self-adhesive breast form and attach it to your chest wall with sticky strips. These strips help the form stay in place comfortably and securely.
- Partial breast prosthesis: This type of prosthesis is also called a shaper or shell. These forms are typically made from lightweight foam or fiberfill, but sometimes heavier silicone is used. You can position them over your chest wall or your breast tissue. They’re designed to balance out the size of your breasts and make them more uniform.
The Women’s Health and Cancer Rights Act (WHCRA) is a law that was passed in 1998. It requires group health insurance companies to cover the cost of both breast mastectomy and breast reconstruction following any mastectomy.
The WHCRA says that a health insurance plan must pay for reconstruction at any point, even years after the mastectomy. The insurance company must also pay for breast prostheses and the treatment of any health complications from your surgery.
However, insurance coverage does not mean low out-of-pocket costs. If you have insurance, talk with your doctor and plan administrator about what you should expect to pay. Your out-of-pocket costs will be based on the array of treatment options your doctor gives you and your specific plan’s coverage.
Medicare covers breast reconstruction, but Medicaid’s coverage varies by state.
Remember that total costs may go beyond the surgery itself. Consider factors like transportation and housing if a family member needs to stay at the hospital with you. You may also need short-term treatments, like physical or occupational therapy.
Your doctor can provide a clear plan for treatment and recovery. This plan can help you understand what services you will need and what they may cost.
Coverage if you don’t have insurance
A mastectomy and breast reconstruction can be costly, but there are programs available to help.
My Hope Chest, for example, is a nonprofit that helps people with breast cancer get reconstruction after a mastectomy.
My Hope Chest is funded by donations and works closely with national breast cancer organizations. Together, they find doctors and other healthcare professionals who want to help people on the My Hope Chest waiting list.
A mastectomy is one possible option for breast cancer treatment. It removes breast tissue and sometimes lymph nodes and chest muscles near the breast.
Some people may have a mastectomy alongside another form of breast cancer treatment, such as radiation or chemotherapy. Your doctor can help you decide whether a mastectomy is right for you, and if it is, which type of mastectomy is best.
The earlier a cancer is detected, the better the options for treatment and recovery. But whatever stage you have, there is a treatment that is right for you.
