Imbruvica (ibrutinib) is a prescription drug that’s used to treat certain kinds of cancer and graft-versus-host disease. Imbruvica comes as an oral tablet, capsule, and suspension (a type of liquid mixture).
Imbruvica is prescribed to treat:
- chronic lymphocytic leukemia and small lymphocytic lymphoma in adults
- Waldenstrom macroglobulinemia in adults
- chronic (long lasting) graft-versus-host disease in adults and children 1 year and older
To learn more about Imbruvica’s uses, see the “Is Imbruvica used for CLL?” and “Is Imbruvica used for other conditions?” sections below.
Imbruvica basics
Imbruvica contains the active ingredient ibrutinib. (An active ingredient is what makes a drug work.) Imbruvica belongs to a group of drugs called kinase inhibitors.
Imbruvica is a brand-name medication. A generic version of the drug isn’t currently available.
Like most drugs, Imbruvica may cause mild or serious side effects. The lists below describe some of the more common side effects. These lists don’t include all possible side effects.
Keep in mind that side effects of a drug can depend on:
- your age
- other health conditions you have
- other medications you take
Your doctor or pharmacist can tell you more about the potential side effects of Imbruvica. They can also suggest ways to help reduce side effects.
Mild side effects
Below is a list of some of the mild side effects Imbruvica can cause. To learn about other mild side effects, talk with your doctor or pharmacist, or read Imbruvica’s prescribing information.
Mild side effects reported in people using Imbruvica varied with the condition being treated. But they included:
- bruising
- cough
- diarrhea and constipation
- dizziness
- fatigue (low energy)
- fever
- headache
- joint pain*
- mild infections, such as a urinary tract infection (UTI) and upper respiratory infection
- mouth sores*
- muscle pain, cramps, and spasm
- nausea
- rash
- difficulty breathing
Mild side effects of many drugs may go away within a few days or a couple of weeks. But if they become bothersome, talk with your doctor or pharmacist.
* For more information about this side effect, see the “Side effect focus” section below.
Serious side effects
Serious side effects from Imbruvica can occur, but they aren’t common. If you have serious side effects, call your doctor right away. But if you think you’re having a medical emergency, call 911 or your local emergency number.
Serious side effects of Imbruvica that have been reported include:
- serious infection, such as severe pneumonia
- low levels of certain blood cells, such as:
- neutrophils, which are a type of white blood cell
- platelets
- red blood cells
- heart problems, such as:
- types of cancer other than those treated by Imbruvica, such as skin cancer
- tumor lysis syndrome (TLS), which is a condition that can occur when your body breaks down cancer cells during treatment
- bleeding*
- allergic reaction*
* For more information about this side effect, see the “Side effect focus” section below.
Side effect focus
Learn more about some of the side effects Imbruvica may cause.
Joint pain
It’s possible that you’ll have joint pain from taking Imbruvica. This side effect usually isn’t severe.
Joint pain was common in people taking the drug for blood cancers in studies. But it wasn’t reported by people who took Imbruvica to treat chronic (long lasting) graft-versus-host disease (cGVHD).
What might help
Talk with your doctor if you have joint pain while taking Imbruvica. They may be able to suggest treatments for pain relief.
Bleeding
Bleeding is a serious side effect that’s possible with Imbruvica treatment. Serious bleeding wasn’t common in studies, but it can be life threatening in rare cases.
Your risk of bleeding while taking Imbruvica may be higher if you take other medications that also increase this risk. These include:
- anticoagulants, such as warfarin (Coumadin) or rivaroxaban (Xarelto)
- antiplatelets, such as aspirin or clopidogrel (Plavix)
It’s important to note that your risk of bleeding from certain surgeries may be higher while you’re taking Imbruvica.
What might help
Call your doctor right away if you have any of the following symptoms of bleeding:
- bloody or black, tar-like stool
- bloody or coffee ground-like vomit
- brown or pink urine
- confusion or changes in speech
- coughing up blood
- severe headache, or a headache that won’t go away
- unmanageable bleeding
- unusual bruising
- weakness
But if your symptoms feel life threatening, call 911 or your local emergency number.
Before taking Imbruvica, tell your doctor about all the medications you take, including any over-the-counter medications (such as aspirin). Your doctor can check for any drug interactions with Imbruvica. Based on what they find, they may decide to change your treatment plan. This may include recommending a medication other than Imbruvica for your condition.
Mouth sores
Mouth sores are a common side effect reported by people taking Imbruvica in studies. These sores can happen anywhere in your mouth. They may feel like a small cut.
Mouth sores were reported by people using Imbruvica for either blood cancers or cGVHD. But they were more common in people with cGVHD.
What might help
Mouth sores from Imbruvica may go away on their own after a few days or weeks. But if you develop mouth sores that are bothersome or won’t go away, call your doctor.
Your doctor may recommend treatments to make you more comfortable. They may also suggest you try a medication other than Imbruvica.
Allergic reactionSome people may have an allergic reaction to Imbruvica. Although allergic reactions weren’t reported in studies of Imbruvica, they can still occur.
Symptoms of a mild allergic reaction can include:
- skin rash
- itchiness
- flushing (temporary warmth, redness, or deepening of skin color)
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include swelling under your skin, typically in your eyelids, lips, hands, or feet. They can also include swelling of your tongue, mouth, or throat, which can cause difficulty breathing.
Call your doctor right away if you have an allergic reaction to Imbruvica. But if you think you’re having a medical emergency, call 911 or your local emergency number.
Costs of prescription drugs can vary depending on many factors. These include what your insurance plan covers and which pharmacy you use.
You can visit the Imbruvica manufacturer’s website to see their support options, including an Imbruvica copay card.
You can also visit Optum Perks to get price estimates of what you’d pay for Imbruvica when using coupons from the site. See the coupon options below. (Note: Optum Perks coupons cannot be used with any insurance copays or benefits.)
If you have questions about how to pay for your prescription, talk with your doctor or pharmacist.
Save on Imbruvica with an Rx coupon from Optum Perks
No membership needed, anyone can use
Search and compare prices for your prescriptionFind the lowest price
Free, easy to use coupon cardDelivered digitally today
Redeem at a local pharmacyAccepted at 64,000+ pharmacies
Enter your information:
Location
47201
Dosage
140mg imbruvica (60 Capsules)
Save money without using insurance
Simply show the Optum Perks coupon at your preferred pharmacy or order online and instantly save up to 80% without using insurance. The coupon doesn't expire, so be sure to save it for refills.
Retail price refers to the manufacturer’s published list price and is up to date as of 3/2023. Retail and discounted prices are U.S.-only and can vary based on region and pharmacy. We cannot guarantee that the discounted price listed here will exactly match the price at your pharmacy. Please contact your pharmacy for the exact price.
Optum Perks and Healthline are subsidiaries of RVO Health.
Pricing source:Perks.optum.com

Your doctor will recommend the dosage of Imbruvica that’s right for you. Below are commonly used dosages, but always take the dosage your doctor prescribes.
Forms and strengths
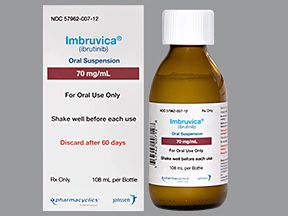
Imbruvica is available as capsules, tablets, and a suspension (a type of liquid mixture) that you swallow.
Here’s a chart showing Imbruvica’s available forms and strengths:
| Imbruvica capsules | Imbruvica tablets | Imbruvica suspension |
| 70 milligrams (mg) | 140 mg | 70 mg per milliliter (mg/mL) |
| 140 mg | 280 mg | |
| 420 mg |
Recommended dosages
For adults and children 12 years and older, the recommended Imbruvica dosage is 420 mg once per day. Your doctor might prescribe Imbruvica capsules or tablets.
To learn more about Imbruvica’s dosage, see this article.
Children’s dosage
In children 1–12 years old, the recommended Imbruvica dosage is 240 mg per meter squared (mg/m2) of body surface area.* Your child’s doctor will tell you exactly how many tablets or capsules your child should take, or how much of the oral suspension to give for each dose.
* Body surface area is a measurement calculated using weight and height.
Questions about Imbruvica’s dosage
Below are answers to a few common questions about taking Imbruvica.
- What if I miss a dose of Imbruvica? If you miss a dose of Imbruvica, try to take it as soon as you remember. But if it’s the next day and you realize you missed a dose, simply skip the missed dose. Then take your next scheduled dose as usual. Do not take more than your regular dose to try and make up for the missed dose.
- Will I need to use Imbruvica long term? What’s the treatment duration of this drug? You’ll likely take Imbruvica long term, unless you have unbearable side effects, or your condition gets worse during treatment. Exactly how long you’ll take the drug depends on your condition and how your body responds to treatment. Your doctor can tell you more about how long you’ll need to take Imbruvica.
- How long does Imbruvica take to work? Imbruvica begins working as soon as you take a dose. But it may take some time before results can be detected on lab tests. In studies, people taking Imbruvica saw a response, on average, between a little over 1 month to about 4.5 months. The length of time varies depending on the condition Imbruvica is prescribed to treat.
Below are answers to some commonly asked questions about Imbruvica.
Is Imbruvica a chemotherapy or immunotherapy drug?
Imbruvica isn’t a chemotherapy drug. Chemotherapy drugs affect cells in your body that are quickly multiplying (making more cells). This includes cancer cells, but it also includes healthy cells. This is why chemotherapy drugs can cause so many side effects.
It’s also not an immunotherapy drug. Immunotherapy drugs work by boosting your own immune system or changing how it works in order to fight cancer cells.
Imbruvica is called a kinase inhibitor. It’s a type of targeted therapy. This treatment targets the specific parts of cancer cells that help them grow and spread.
For more information on how Imbruvica works, see “How does Imbruvica work?” below.
Are reviews available from people who’ve taken Imbruvica?
If you’d like to learn more about what people who’ve taken Imbruvica have to say, talk with your doctor. They may be able to provide you with reviews and other information from people who have had Imbruvica treatment.
How does Imbruvica work? What’s its half-life?
Imbruvica’s mechanism of action (how it works) is to target and block a certain enzyme (type of protein). The enzyme in your body that Imbruvica targets is called Bruton’s tyrosine kinase (BTK).
Blocking BTK keeps cancer cells from growing. This is how Imbruvica treats certain types of cancer.
Blocking BTK also stops certain immune system cells from working. This is how Imbruvica works to treat chronic (long lasting) graft-versus-host disease (cGVHD).
Imbruvica has a
If you’d like to learn more about how Imbruvica works, talk with your doctor or pharmacist.
Are there alternatives for Imbruvica?
Yes, there are alternatives to Imbruvica that can treat leukemia, lymphoma, or chronic (long lasting) graft-versus-host disease (cGVHD).
A few examples include:
- bendamustine (Treanda)
- infliximab (Remicade)
- rituximab (Rituxan)
- venetoclax (Venclexta*)
Some may be a better fit for you than others. If you’re interested in finding an alternative to Imbruvica, talk with your doctor. They can tell you about the best treatment option for your condition.
* To view a detailed comparison of Imbruvica and Venclexta, see this article.
Can I take Imbruvica if I’m having surgery?
Maybe. Talk with your doctor if you plan on having any type of surgery, including dental procedures, while taking Imbruvica.
Keep in mind that Imbruvica can increase your risk of bleeding. So your doctor may have you pause from taking Imbruvica about 3 to 7 days before your surgery. This helps prevent severe bleeding during your procedure. But you should not stop taking Imbruvica unless your doctor specifically tells you to do so.
Questions for your doctorYou may have questions about Imbruvica and your treatment plan. It’s important to discuss all your concerns with your doctor.
Here are a few tips that might help guide your discussion:
- Before your appointment, write down questions such as:
- How will Imbruvica affect my body, mood, or lifestyle?
- Bring someone with you to your appointment if doing so will help you feel more comfortable.
- If you don’t understand something related to your condition or treatment, ask your doctor to explain it to you.
Remember, your doctor and other healthcare professionals are available to help you. And they want you to get the best care possible. So, don’t be afraid to ask questions or offer feedback on your treatment.
Yes, Imbruvica is prescribed to treat chronic lymphocytic leukemia (CLL) in adults. This includes people who have CLL with a 17p deletion. (This is a change in your chromosomes, which make up your genes.)
CLL is a type of leukemia, which is a cancer that affects your blood and bone marrow. With CLL, your body makes abnormal lymphocytes (a type of white blood cell) in large numbers.
CLL is a slow-growing cancer that can take years to get worse. Many people with CLL don’t show symptoms for several years. Over time, CLL can lead to problems such as a low level of red blood cells and platelets.
Imbruvica works to treat CLL by targeting and blocking a certain enzyme (a type of protein) in your body. Blocking this enzyme stops cancer cells from growing.
In addition to CLL, Imbruvica also treats other conditions. See “Is Imbruvica used for other conditions?” just below for details.
Imbruvica is prescribed to treat chronic lymphocytic leukemia (CLL) and other conditions, such as:
- Small lymphocytic leukemia (SLL) in adults. This is a type of leukemia (blood cancer) that happens in your lymph nodes (a part of your immune system). Like CLL, it causes your body to make abnormal lymphocytes (a type of white blood cell) in large numbers. SLL is a slow-growing cancer that can take years to get worse. Imbruvica may be used to treat SLL in people who do or do not have a 17p deletion (a change in your chromosomes, which make up your genes).
- Waldenstrom macroglobulinemia (WM) in adults. WM is a rare type of non-Hodgkin’s lymphoma that affects your plasma cells (a type of white blood cell). It causes your body to make too much of an immune system protein called IgM. This makes your blood thicker than usual, and your organs have a hard time working properly because of this.
- Chronic (long lasting) graft-versus-host disease (cGVHD). cGVHD can happen after you receive a stem cell transplant. With cGVHD, the transplanted cells attack your own body. Imbruvica is only used to treat cGVHD in people who’ve tried another treatment, but their condition got worse. Imbruvica can be prescribed for cGVHD in adults and in children 1 year and older.
See “Is Imbruvica used for CLL?” above for details about Imbruvica’s use for this type of cancer.
Imbruvica and Venclexta are both used to treat chronic lymphocytic leukemia (CLL) and small lymphocytic leukemia (SLL). But they’re used to treat some different conditions as well.
Imbruvica and Venclexta both belong to a group of medications called targeted therapies. But they contain different active drugs and work in slightly different ways. Because of this, they may cause different side effects.
To learn more about how these drugs compare, see this article. Also, talk with your doctor about which drug is best for you.
Your doctor will explain how you should take Imbruvica. They’ll also explain how much to take and how often. Be sure to follow your doctor’s instructions.
Taking Imbruvica
Imbruvica comes as capsules, tablets, and an oral suspension. Each form is swallowed.
You should take Imbruvica with a glass of water. This includes the oral suspension form; be sure to drink a glass of water after swallowing a dose.
The suspension comes with oral dosing syringes to help you give the correct dose. It also comes with instructions for how to measure and give a dose.
Taking Imbruvica with other drugs
Depending on the condition it’s used to treat, Imbruvica may be used together with other drugs. Talk with your doctor if you have questions about taking Imbruvica with other drugs.
Questions about taking Imbruvica
Below are answers to a couple of common questions about taking Imbruvica.
- Can Imbruvica be chewed, crushed, or split? No, you should not chew, crush, or split Imbruvica capsules or tablets. Imbruvica capsules and tablets should be swallowed whole. If you have difficulty swallowing capsules or tablets, check out this article. Or talk with your pharmacist or doctor. They can tell you whether you could take the Imbruvica oral suspension instead.
- Should I take Imbruvica with food? Imbruvica may be taken with or without food. That said, you should take your dose with a glass of water.
Ask your doctor about the benefits and risks of treatment before you start taking Imbruvica. Tell them about all your health conditions and any medications you’re currently taking.
These and other considerations are described below.
Interactions
Taking a medication with certain vaccines, foods, and other things can affect how the medication works. These effects are called interactions.
Before taking Imbruvica, be sure to tell your doctor about all medications you take, including prescription and over-the-counter types. Also, describe any vitamins, herbs, or supplements you use. Your doctor or pharmacist can tell you about any interactions these items may cause with Imbruvica.
Interactions with drugs or supplements
Imbruvica can interact with several types of drugs, including:
- blood thinners, such as:
- apixaban (Eliquis)
- rivaroxaban (Xarelto)
- warfarin (Coumadin)
- certain antibiotics, such as clarithromycin (Biaxin)
- certain antiepileptic drugs, such as phenytoin (Dilantin) and carbamazepine (Tegretol)
- certain antifungal drugs, such as:
- itraconazole (Sporanox)
- ketoconazole
- voriconazole (Vfend)
- certain HIV drugs, such as ritonavir (Norvir) and saquinavir (Invirase)
This list does not contain all types of drugs that may interact with Imbruvica. Your doctor or pharmacist can tell you more about these interactions and any others that may occur with Imbruvica.
Other interactions
You should avoid drinking grapefruit juice or eating grapefruit while you’re taking Imbruvica. You should also avoid Seville oranges, which are sometimes called bitter oranges.
Both fruits can increase Imbruvica levels in your body, increasing your risk of side effects.
Talk with your doctor before you begin taking Imbruvica if you usually consume grapefruit or Seville oranges.
Warnings
Imbruvica may not be right for you if you have certain medical conditions or other factors that affect your health. Talk with your doctor about your health history before you take Imbruvica. Factors to consider include those in the list below.
- Bleeding problems. Imbruvica treatment can increase your risk of bleeding. While rare, this can be serious or even life threatening. If you already have a bleeding problem and take Imbruvica, it can increase your risk of this side effect. Your doctor can help determine if the drug is safe for you to take or if a different medication would be better for you.
- Heart rhythm problems. Taking Imbruvica can cause problems with your heart rhythm, though this is rare. If you already have a heart rhythm problem, you may be at higher risk of this side effect. Your doctor can help determine if the drug is safe for you or if a different medication would be better.
- Heart failure or being at risk of heart disease. Imbruvica treatment may increase your risk of heart failure. If you already have heart failure, you may be at higher risk. You may also be at higher risk of this side effect if you have a condition that increases your risk of heart disease. This includes diabetes, high cholesterol, or high blood pressure. Your doctor can help determine if the drug is safe for you or if a different medication would be better.
- Current infection. Taking Imbruvica can put you at higher risk of infection. If you currently have an infection, be sure to tell your doctor before you start taking Imbruvica. They may want you to wait for your infection to clear before you begin treatment.
- Liver problems. People with severe liver problems should not take Imbruvica. This is because your liver breaks down and gets rid of the drug after you take a dose. Taking Imbruvica when you have severe liver problems could cause levels of the drug to build up in your body. This can increase your risk of side effects. It’s usually safe for people with mild liver problems to use Imbruvica. But your doctor may monitor your liver health closely during treatment. Talk with your doctor about whether this drug is safe to take if you have liver problems.
- Recent or planned surgery. Imbruvica can increase your risk of bleeding. Because of this, your doctor may have you wait to start taking it if you’ve recently had or plan to have surgery. Your doctor can give you more information on when it’s safe for you to take Imbruvica based on your surgery plan.
- Allergic reaction. If you’ve had an allergic reaction to Imbruvica or any of its ingredients, you should not take Imbruvica. Ask your doctor what other medications are better options for you.
Imbruvica and alcohol
There isn’t a known interaction between consuming alcohol and taking Imbruvica. But it’s always best to check with your doctor about how much alcohol is safe for you based on your health and treatment plan.
Pregnancy and breastfeeding
It’s recommended that you do not take Imbruvica while pregnant or breastfeeding.
If you’re able to become pregnant, your doctor will order a pregnancy test. They’ll confirm it’s negative before prescribing Imbruvica to you. While taking Imbruvica, you should use an effective form of birth control. And you should keep using it for at least 1 month after your last dose of Imbruvica.
You should also avoid breastfeeding while taking Imbruvica and for at least 1 week after your last dose. This is because the drug may cause serious side effects in a child who is breastfed.
Talk with your doctor about the safety of taking Imbruvica while you’re pregnant or breastfeeding.
Do not take more Imbruvica than your doctor prescribes. Taking more than this can lead to serious side effects.
What to do in case you take too much Imbruvica
Call your doctor if you think you’ve taken too much Imbruvica. You can also call 800-222-1222 to reach America’s Poison Centers or use its online resource. But if you have severe symptoms, immediately call 911 (or your local emergency number) or go to the nearest emergency room.
Ask your doctor for information about the risks and benefits of taking Imbruvica for your condition. Here are a few questions you can ask:
- What should I expect when starting treatment with Imbruvica?
- How will I know if Imbruvica is working for me?
- How long will I need to take Imbruvica?
- Do I need to stop taking Imbruvica if I get an infection?
To learn more about Imbruvica, see these articles:
- Dosage Details for Imbruvica
- Imbruvica and Cost: What You Need to Know
- Side Effects of Imbruvica: What You Need to Know
To get information on different conditions and tips for improving your health, subscribe to any of Healthline’s newsletters. You may also want to check out the online communities at Bezzy. It’s a place where people with certain conditions can find support and connect with others.
Q:
Will I need to have lab tests done while I’m taking Imbruvica? If so, what kind of tests and how often?
AnonymousA:
Yes, you will. People taking Imbruvica need to have blood tests done monthly.
Depending on your health history, you may need blood tests more often. And other tests may be needed if you have certain side effects. These other tests could include an electrocardiogram (ECG), which checks how your heart is working.
If you want to know more about tests you may need while taking Imbruvica, talk with your doctor before and during treatment.
The Healthline Pharmacist TeamAnswers represent the opinions of our medical experts. All content is strictly informational and should not be considered medical advice.Disclaimer: Healthline has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.